13.3
Impact Factor
Theranostics 2025; 15(3):1122-1134. doi:10.7150/thno.101358 This issue Cite
Research Paper
Drug repositioning of mesalamine via supramolecular nanoassembly for the treatment of drug-induced acute liver failure
1. KU-KIST Graduate School of Converging Science and Technology, Korea University, Seoul 02841, Republic of Korea.
2. Medicinal Materials Research Center, Biomedical Research Division, Korea Institute of Science and Technology (KIST), Seoul 02792, Republic of Korea.
3. Department of Life Sciences, Korea University, Seoul 02841, Republic of Korea.
4. Division of Bio-Medical Science and Technology, KIST School, Korea University of Science and Technology, Seoul 02792, Republic of Korea.
5. College of Pharmacy, Graduate School of Pharmaceutical Sciences, Ewha Womans University, Seoul 03760, Republic of Korea.
6. College of Pharmacy, Graduate School of Pharmaceutical Sciences, Kyung Hee University, Seoul 02453, Republic of Korea.
Abstract
Rationale: Acute liver failure (ALF) is characterized by rapid hepatic dysfunction, primarily caused by drug-induced hepatotoxicity. Due to the lack of satisfactory treatment options, ALF remains a fatal clinical disease, representing a grand challenge in global health.
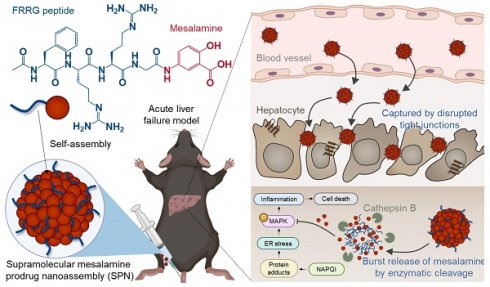
Methods: For the drug repositioning to ALF of mesalamine, which is clinically approved for the treatment of inflammatory bowel disease (IBD), we propose a supramolecular prodrug nanoassembly (SPNs). Mesalamine is modified with a functional peptide of the FRRG sequence. The resulting mesalamine prodrugs form nanoassemblies solely through intermolecular interactions, ensuring high drug loading capacity and reducing the potential toxicity associated with the carrier materials of conventional nanoparticle systems.
Results: In acetaminophen (APAP)-induced ALF mouse models, the SPNs predominantly accumulate in injured target tissues owing to the nanoparticles' propensity to target the liver. Subsequently, cathepsin B overexpressed in hepatocytes by drug-induced inflammation triggers the release of mesalamine from the nanoassemblies via enzymatic cleavage, resulting in remarkable therapeutic efficacy. Meanwhile, nonspecific drug release in healthy cells is inhibited due to their relatively lower cathepsin B expression, which helps prevent the exacerbation of the ALF by minimizing adverse events related to drug exposure.
Conclusions: This study provides valuable insights into designing rational nanomedicine for repurposing mesalamine in ALF treatment, potentially inspiring further research to discover effective and safe therapeutic options for patients.
Keywords: Acute liver injury, Supramolecular assembly, Prodrug, Mesalamine, Drug repositioning
 Global reach, higher impact
Global reach, higher impact