13.3
Impact Factor
Theranostics 2025; 15(3):965-992. doi:10.7150/thno.102964 This issue Cite
Review
RNA nanotherapeutics for hepatocellular carcinoma treatment
1. The Comprehensive Cancer Centre of Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University and Clinical Cancer Institute of Nanjing University, Nanjing 210008, China.
2. Department of Hepatobiliary Surgery, Academician (Expert) Workstation, Affiliated Hospital of North Sichuan Medical College, Nanchong 637600, China.
3. School of Life Sciences, Jiangsu University, Zhenjiang 212013, China.
4. Department of Medical Oncology, The First Affiliated Hospital of Bengbu Medical University, Bengbu 233004, China.
5. Department of General Surgery Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School Nanjing University, Nanjing 210008, China.
6. Center for Nanomedicine and Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA 02115, USA.
7. Department of Urology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA 02115, USA.
# These authors made equal contributions to this work.
Received 2024-8-29; Accepted 2024-11-22; Published 2025-1-1
Abstract
Hepatocellular carcinoma (HCC) remains a leading cause of cancer-related mortality worldwide, particularly due to the limited effectiveness of current therapeutic options for advanced-stage disease. The efficacy of traditional treatments is often compromised by the intricate liver microenvironment and the inherent heterogeneity. RNA-based therapeutics offer a promising alternative, utilizing the innovative approach of targeting aberrant molecular pathways and modulating the tumor microenvironment. The integration of nanotechnology in this field, through the development of advanced nanocarrier delivery systems, especially lipid nanoparticles (LNPs), polymer nanoparticles (PNPs), and bioinspired vectors, enhances the precision and efficacy of RNA therapies. This review highlights the significant progress in RNA nanotherapeutics for HCC treatment, covering micro RNA (miRNA), small interfering RNA (siRNA), message RNA (mRNA), and small activating RNA (saRNA) mediated gene silencing, therapeutic protein restoration, gene activation, cancer vaccines, and concurrent therapy. It further comprehensively discusses the prevailing challenges within this therapeutic landscape and provides a forward-looking perspective on the potential of RNA nanotherapeutics to transform HCC treatment.
Keywords: RNA nanotherapeutics, Gene regulation, Protein restoration, Gene activation, Hepatocellular carcinoma
Introduction
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy and a leading cause of cancer-related deaths worldwide, with a five-year survival rate of approximately 18% due to asymptomatic progression and late detection [1-3]. Current treatments for HCC, including surgical resection, liver transplantation, local ablative therapies, and systemic treatments such as chemotherapy and targeted therapy, are often ineffective, especially at advanced stages [4-7]. Fewer than 20% of patients are eligible for surgery, systemic chemotherapy offers limited benefits with significant toxicity, and targeted agents provide only modest survival improvements, frequently hindered by drug resistance and adverse effects. Additionally, tumor heterogeneity and the unique liver microenvironment promote drug resistance and reduce therapeutic efficacy by shielding cancer cells and rapidly metabolizing drugs [8-11]. These issues highlight the urgent need for novel therapeutic strategies for HCC.
RNA-based therapeutics have emerged as a promising strategy for HCC treatment due to their ability to modulate gene expression directly associated with tumor progression, thus minimizing off-target effects and toxicity. RNA therapeutics, including microRNA (miRNA), small interfering RNA (siRNA), messenger RNA (mRNA), and small activating RNA (saRNA), offer a novel strategy for specifically modulating gene expression linked to tumorigenesis, facilitating precise and effective treatment [12-14]. However, the clinical application of RNA therapeutics faces significant challenges due to the instability of RNA molecules, susceptibility to degradation by nucleases, poor cellular uptake, and potential immunogenicity.
Nanotechnology has provided solutions to many of these limitations by enabling the development of nanocarriers that protect and deliver RNA molecules effectively to tumor sites. Nanocarriers such as lipid nanoparticles (LNPs), polymeric nanoparticles (PNPs), and bioengineered vectors enhance the stability, bioavailability, and targeted delivery of RNA molecules [15-18]. LNPs, for example, protect RNA from enzymatic degradation and facilitate efficient cellular uptake, as demonstrated in the delivery of mRNA vaccines during the COVID-19 pandemic [19]. Similarly, PNPs and extracellular vesicles (EVs) can be engineered to improve delivery efficiency, reduce off-target effects, and modulate the tumor microenvironment (TME) to enhance therapeutic outcomes. For example, by functionalizing the nanoparticle surface with tumor-specific ligands or antibodies, the nanoparticles can selectively bind to receptors overexpressed on HCC cells, such as glypican-3 (GPC3) or transferrin receptors [20, 21]. This targeted binding facilitates increased accumulation of the therapeutic RNA at the tumor site, improving efficacy while reducing systemic toxicity and side effects. Additionally, this strategy allows for controlled release of the RNA payload in response to specific stimuli within the TME, such as pH changes or enzymatic activity, further enhancing therapeutic precision.
Therefore, RNA nanotherapeutics, which involve nanocarrier-encapsulated RNA therapeutics, have shown significant progress in HCC treatment. The first approved siRNA drug, Patisiran, which is formulated into LNPs, effectively treats hereditary transthyretin-mediated amyloidosis, and its liver-specific delivery system also shows potential for liver cancer treatment [22]. TKM-PLK consists of siRNA designed to silence PLK1 encapsulated in LNPs, and is undergoing clinical trials for HCC treatment [23]. miRNA-based therapies have also entered clinical trials, with MRX34 being the first therapy to target liver cancer [24]. saRNA has also demonstrated promising potential in liver cancer therapy; the first saRNA drug to enter clinical trials, MTL-CEBPA (NCT02716012), has shown excellent safety and therapeutic prospects when combined with TKIs, potentially becoming the first RNA drug for HCC treatment [25]. Moreover, our group was the first to demonstrate the therapeutic potential of restoring tumor suppressor function using RNA-based therapeutics in liver cancer, initially demonstrating that p53 restoration sensitizes p53-deficient cancers to mTOR inhibition and subsequently showing that p53 restoration enhances anti-tumor immunity [26]. More recently, we reported a PNP platform for delivering p53 mRNA, which directly inhibited liver cancer growth and enhanced anti-tumor immune responses by modulating the immune microenvironment. When this mRNA delivery system was combined with immune checkpoint inhibitors such as anti-PD-1, it significantly enhanced anti-tumor effects, surpassing the efficacy of anti-PD-1 therapy alone [27]. These developments underscore the versatility of RNA nanotherapeutics, which hold considerable promise for overcoming the challenges of conventional HCC therapies through targeted, potent, and personalized approaches.
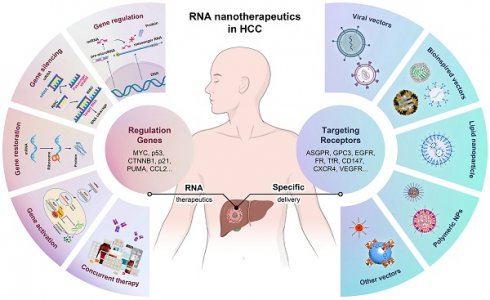
The rationale for using nanotechnology-enhanced RNA therapeutics in HCC allows for precise modulation of genes involved in hepatocarcinogenesis, offering potential for more effective and personalized treatment options [28-30]. In this review, as shown in Figure 1, we summarize the concept of RNA nanotherapeutics in HCC, showcasing key approaches such as gene regulation, gene silencing, gene restoration, gene activation, and concurrent therapies. Different RNA types, including siRNA, miRNA, and mRNA, are being utilized to target genes involved in HCC progression. We also illustrate the various delivery vectors, such as bioinspired vectors, LNPs, PNPs, and other vectors, used to target receptors overexpressed on HCC cells (e.g., ASGPR, GPC3, EGFR, and CXCR4). The convergence of RNA-based strategies and nanotechnology not only paves the way for overcoming the multifaceted resistance observed in HCC treatment, but also aligns with the overarching goal of precision medicine in oncology. This review explores the current state and prospects of RNA-based therapies in treating HCC, highlighting the advances, challenges, and potential of this emerging field, and providing new directions for designing precise, effective, and personalized RNA nanomedicines.
Schematic of RNA nanotherapeutics in HCC treatment. This schematic illustrates the multifaceted approach of RNA-based therapies in HCC, including gene silencing, regulation, restoration, activation, and concurrent therapy. The left side highlights various RNA strategies, including gene silencing, gene regulation, gene restoration, gene activation, and concurrent therapy, targeting critical genes such as MYC, p53, and CTNNB1. The right side shows the advanced nanocarrier systems used for a specific delivery, including viral vectors, bioinspired vectors, LNPs, PNPs, and other NPs, to target HCC receptors like ASGPR, GPC3, and EGFR, enhancing the precision of RNA delivery to HCC.
Types and mechanisms of RNA therapeutics
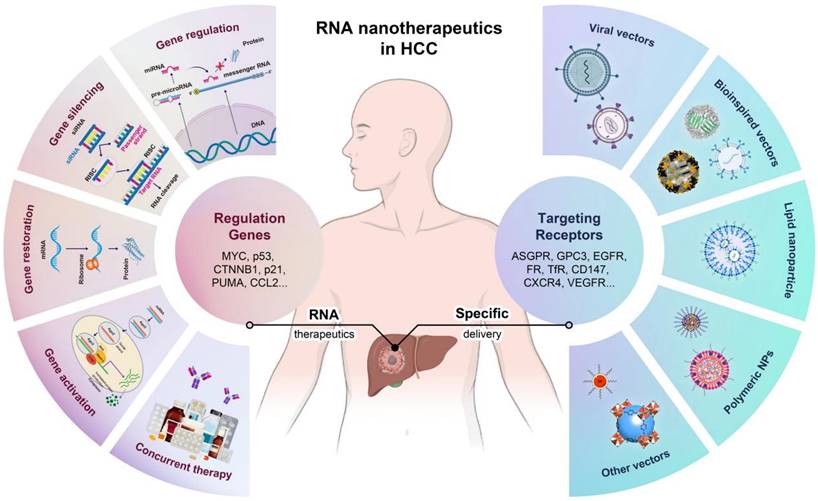
RNA therapies have emerged as a revolutionary force in modern medicine, distinguished by their precision, versatility, and safety, making them ideal for treating a wide array of diseases, from genetic disorders to cancer. These therapies precisely target specific genes or pathways, significantly reducing potential side effects by affecting only disease-related processes. Diverse RNA molecules, including miRNA, siRNA, mRNA, and saRNA, provide various mechanisms for gene silencing, expression enhancement, or protein replacement (Figure 2), allowing RNA therapies to adapt to various medical conditions, from genetic diseases to cancer. Moreover, the rapid development cycle of RNA molecules enables swift responses to emerging health challenges, such as viral outbreaks. Importantly, unlike some gene therapies that may integrate into the genome and potentially cause mutations, RNA therapies do not integrate into the host DNA, thereby avoiding the risks of long-term genetic alterations and enhancing their safety profile [31]. Additionally, RNA therapies allow for the control of gene expression duration and intensity, enabling personalized treatment approaches that ensure efficacy while minimizing risks [32]. Overall, these characteristics underscore the transformative potential of RNA therapies in advancing the capabilities of precision medicine.
MicroRNA (miRNA)
miRNA is a class of small non-coding RNA molecules that play a critical role in gene expression regulation through the RNA interference pathway. Typically around 22 nucleotides in length, miRNAs are initially transcribed from DNA as longer primary transcripts (pri-miRNAs) and are then processed into shorter precursor miRNAs (pre-miRNAs) in the nucleus. The pre-miRNA is exported to the cytoplasm, which is further processed by the Dicer enzyme into mature miRNA duplexes. One strand of the duplex, the mature miRNA, is incorporated into the RNA-induced silencing complex (RISC), guiding the complex to complementary mRNA targets, thereby inhibiting their expression through mRNA degradation or translational repression [33]. miRNAs are crucial for maintaining cellular homeostasis, and their dysregulation is associated with various diseases, including cancer, cardiovascular diseases, and neurodegenerative disorders [34]. This makes them valuable targets for research as diagnostic and prognostic biomarkers and therapeutic agents. In oncology, specific miRNAs differentiate tumor types based on their expression profiles. Therapeutically, miRNAs can be manipulated to inhibit tumor growth by modulating the expression of oncogenes or tumor suppressor genes [35].
The use of miRNA for therapy offers several advantages, including high specificity and the ability to simultaneously regulate multiple targets involved in disease pathways, potentially leading to more comprehensive and effective treatment outcomes. Their small size and natural presence in the body reduce the likelihood of adverse immune reactions, which is a significant advantage over other therapeutic agents. However, miRNA-based therapies also face challenges. Delivering miRNAs to specific cells and tissues without degradation remains a major obstacle due to their instability in the bloodstream and the general inefficiency of existing delivery systems [36]. Additionally, miRNAs may inadvertently regulate unintended mRNA targets, leading to off-target effects [37]. Given their complex regulatory roles in various cellular processes, altering miRNA levels may have widespread and unpredictable impacts on other biological processes.
The miRNA research continues to expand rapidly, offering new insights into gene regulation and cellular function. The development of novel delivery systems, such as NP-based carriers, and the refinement of miRNA mimics and inhibitors, are advancing the clinical application of miRNAs. As our understanding of miRNAs deepens and technology progresses, miRNAs are expected to become a central component of targeted therapeutic strategies, offering solutions for diseases that currently lack effective treatments.
Types and mechanisms of RNA-based therapeutics. siRNA and miRNA induce gene silencing through mRNA cleavage or translational inhibition, while mRNA and saRNA enhance protein production by direct translation or transcriptional activation.
Small interfering RNA (siRNA)
siRNA plays a crucial role in molecular biology and therapeutics, primarily through its function in the RNA interference (RNAi) pathway, which controls gene expression by silencing specific genes. Typically 20-25 nucleotides long, siRNAs are double-stranded molecules with two-nucleotide overhangs, formed from longer dsRNA precursors by the Dicer enzyme [38]. The guide strand of siRNA is incorporated into the RISC, which binds to complementary mRNA, leading to its cleavage and degradation, thus silencing the gene.
In research, siRNAs are invaluable tools for studying gene function by selectively silencing genes. Therapeutically, siRNAs are being developed to treat conditions such as viral infections, cancer, and genetic disorders by targeting disease-related genes [39, 40]. Their high specificity allows them to minimize off-target effects compared to traditional drugs. However, challenges remain in delivering siRNAs effectively into cells while maintaining their stability in the bloodstream [41]. There is also a risk of siRNAs triggering immune responses, as they can resemble viral RNA.
Despite these challenges, significant progress has been made in the clinical development of siRNA-based gene therapies. Techniques to improve siRNA stability and delivery, such as chemical modifications and NP carriers, have advanced to clinical trials. For example, Patisiran, a siRNA therapeutic targeting transthyretin, has been approved by the FDA for treating hereditary transthyretin-mediated amyloidosis, marking a significant milestone in RNAi therapy [42]. In summary, siRNA technology offers a powerful means of gene therapy, with the potential to precisely alter gene expression and address diseases at their genetic roots.
Messenger RNA (mRNA)
mRNA therapy is a revolutionary approach in medicine, leveraging the body's cellular machinery to produce therapeutic proteins. This strategy has significantly advanced research and clinical applications, particularly in addressing diseases rooted in genetic abnormalities or protein dysfunction [43-45]. Although the concept of using mRNA as a therapeutic tool emerged decades ago, it was only in the late 20th and early 21st centuries that technological breakthroughs enabled the development of stable and effective mRNA therapies [46]. Early challenges, such as mRNA instability and high immunogenicity, initially hindered its therapeutic potential [47]. However, advancements in modified nucleotides have reduced these issues, paving the way for mRNA's use in vaccines and protein replacement therapies. mRNA, a single-stranded molecule, carries genetic instructions from DNA to ribosomes, where it directs protein synthesis. Therapeutically, synthetic mRNA is designed to encode specific proteins, and once delivered, it utilizes the cell's machinery to produce these proteins. This technology's flexibility has led to its exploration in vaccines, cancer immunotherapy, and genetic disorder treatments. The success of mRNA vaccines in combating COVID-19, particularly through the Pfizer-BioNTech and Moderna vaccines, highlights its potential [48]. Beyond infectious diseases, mRNA is being investigated for its ability to stimulate immune responses against cancer by encoding tumor antigens, and in genetic disorders [49-51], it serves as a template for producing missing or defective proteins.
A key advantage of mRNA therapy is its safety, as mRNA does not integrate into the host genome, eliminating the risk of insertional mutagenesis associated with some gene therapies. mRNA therapy is also highly flexible, allowing for rapid design and manufacturing, which is particularly beneficial in responding to emerging health threats and pandemics. However, mRNA therapy also faces challenges, primarily related to delivery and stability [52]. mRNA molecules are inherently unstable and prone to degradation, requiring sophisticated delivery systems to protect the mRNA and ensure its effective uptake and expression in target cells. Common strategies include encapsulating mRNA in LNPs to enhance cellular uptake and protect it from degradation. While mRNA's immunogenicity is advantageous in vaccine applications, it can be a drawback in other therapeutic contexts, potentially triggering unwanted immune responses [53].
The success of mRNA COVID-19 vaccines has catalyzed further research into broader applications. Continued research is focused on refining mRNA modifications and delivery systems to enhance the safety, efficacy, and durability of mRNA therapies [54]. In summary, mRNA therapy presents a dynamic and adaptable platform in modern medicine, offering significant potential across a broad spectrum of diseases. As understanding and technologies improve, mRNA is set to become a cornerstone in the future of therapeutic strategies.
Small activating RNA (saRNA)
saRNA represents an innovative class of RNA therapies distinct from the more common silencing RNA. Unlike siRNA, which is designed to downregulate gene expression, saRNA is engineered to upregulate gene expression [55, 56]. This unique capability opens new avenues for therapeutic intervention, particularly in cases where gene activation is required. The concept of saRNA emerged from the RNAi field, which traditionally focused on gene silencing. The discovery that RNA could also be used to enhance gene expression significantly altered the initial understanding of RNAi [57]. Early studies showed that double-stranded RNA could target promoters and enhance gene transcription, a phenomenon first observed in plants and later confirmed in mammalian cells. This discovery led to the identification and development of saRNA as a new tool for gene activation.
saRNAs are short, double-stranded RNA molecules (20-25 nucleotides) that target promoter regions to recruit RNAi machinery and transcription factors, enhancing gene transcription [58]. This unique ability makes saRNA valuable for diseases requiring gene activation, such as liver diseases and metabolic disorders, by promoting the production of proteins that reverse liver damage or regulate metabolic pathways [59]. saRNA also holds potential in regenerative medicine, such as activating genes involved in cell growth and differentiation [60, 61].
Compared to other RNAi technologies, the clinical development of saRNA is still in its early stages. However, promising preclinical studies have laid the foundation for initial clinical trials. For example, an saRNA designed to activate the CEBPA gene, a crucial regulator in bone marrow biology, is being investigated for treating liver cancer and certain hematologic disorders [62, 63]. This reflects the broad potential of saRNA in treating a wide range of diseases that require gene activation for effective therapy.
saRNA's ability to selectively activate genes broadens the therapeutic landscape beyond traditional silencing approaches. It can be synthesized using existing RNAi technology platforms, facilitating rapid development. However, challenges remain: ensuring consistent and efficient gene activation requires precise targeting [64]. Like other RNA therapies, saRNA also faces delivery challenges, requiring protection from degradation and effective cellular uptake mechanisms to reach its target sites in the genome [65]. Therefore, saRNA represents a promising yet still evolving technology in RNA therapies. With its unique ability to activate gene expression, saRNA has the potential to play a significant role in treating a wide range of genetic and acquired diseases. Continued research and development are essential to overcoming current limitations and fully realizing the clinical potential of this innovative therapy.
Nanotechnology improves RNA delivery
Effective RNA therapy depends on the precise and stable delivery of RNA to target cells and its successful release from lysosomes or endosomes. NPs play a critical role in protecting RNA molecules from degradation in the bloodstream, enhancing their stability and lifespan. These NPs can be functionalized with ligands or antibodies on their surface to recognize specific cellular receptors, creating delivery systems tailored to target specific tissues or cell types. This targeted delivery improves RNA uptake by diseased cells while minimizing off-target effects. Moreover, NPs can be engineered to respond to specific stimuli, ensuring controlled release in the target environment. This approach maximizes therapeutic efficacy while reducing side effects. Additionally, NPs offer multifunctionality, integrating therapeutic and diagnostic capabilities within a single platform, enabling real-time monitoring of treatment and disease progression [66]. The combination of RNA therapies with advanced NP delivery systems marks a significant advancement in precision medicine, offering highly effective, customizable, and safe treatment options.
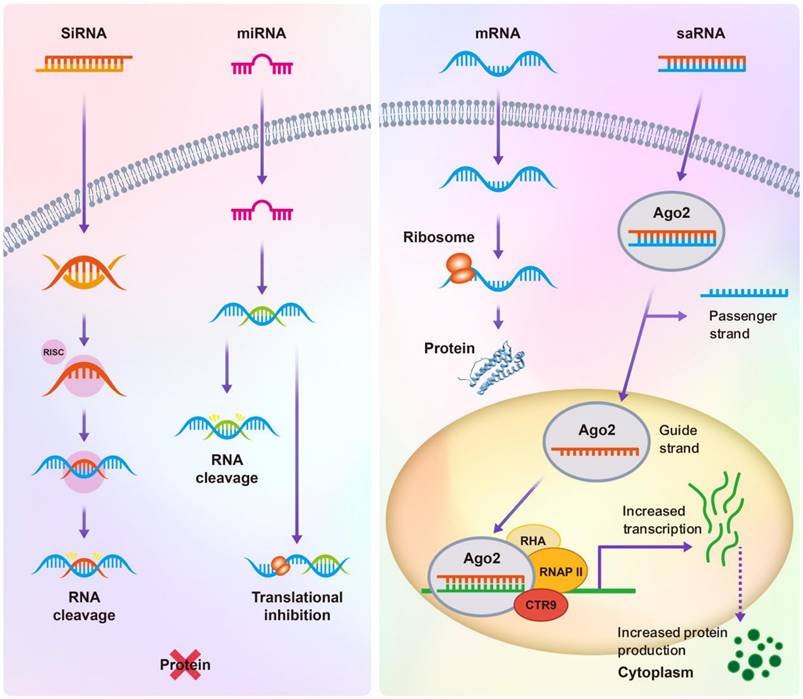
The efficient delivery of RNA molecules relies on advanced nanocarrier systems, each employing unique mechanisms to ensure stability and specificity. As shown in the Figure 3, various RNA delivery vectors have been developed to optimize therapeutic efficacy. Gene delivery vectors include viral options like lentiviruses, and adeno-associated viruses (AAV), which are efficient but may trigger immune responses and pose risks of insertional mutagenesis [67]; Non-viral alternatives include bioinspired NPs such as virus-like particles (VLPs), nanocages, EVs, and exosomes [68], which mimic biological structures to enhance biocompatibility. LNPs are particularly noteworthy in RNA therapy, providing protection and improving cellular uptake efficiency, while PNPs made from materials like PLGA allow for controlled, stimulus-responsive release [69, 70]. Other innovative materials like metal-organic frameworks (MOFs) and quantum dots (QDs) offer unique properties for RNA delivery and therapeutic tracking [71].
Viral vectors
Viral vectors are powerful tools in gene therapy, widely used for RNA delivery due to their inherent ability to enter cells and achieve high levels of gene expression. These vectors exploit the natural mechanisms viruses have evolved to introduce their genetic material into host cells. Viral vectors are engineered to be replication-deficient, meaning they cannot reproduce within the host cell, thereby significantly reducing their pathogenicity [72-74]. Commonly used viral vectors for RNA delivery include lentiviruses, adenoviruses, AAV, and retroviruses, each with unique characteristics suitable for specific applications. For example, lentiviruses integrate into the host genome, allowing long-term expression in both dividing and non-dividing cells, while adenoviruses achieve high transduction efficiency but provide only transient expression as they do not integrate into the genome.
Viral vectors have driven the development of numerous clinical applications. For example, AAV vectors are used in FDA-approved therapies like Luxturna™ for inherited retinal disease and Zolgensma™ for spinal muscular atrophy [75, 76], demonstrating their potential in treating genetic disorders. Lentiviral vectors have been successful in CAR-T cell therapies for cancer, where they modify T cells to target specific cancer cells [77]. Research continues to explore the use of viral vectors in a wide range of conditions, including infectious diseases and metabolic disorders.
Despite their efficacy in delivering genetic material and achieving substantial gene expression, viral vectors come with significant challenges [78]. Immunogenicity is a major issue, as the body's immune response to viral proteins can cause inflammation and reduce the therapy's effectiveness, particularly with repeated administration. Safety concerns also arise from the risk of insertional mutagenesis, especially with vectors like lentiviruses and retroviruses that integrate into the host genome. If these vectors insert themselves in a way that disrupts tumor suppressor genes or activates oncogenes, there is a potential cancer risk. Moreover, producing viral vectors is a complex and expensive process, demanding rigorous manufacturing standards to ensure safety and effectiveness.
Overview of RNA delivery vectors and their underlying mechanisms. Viral vectors, such as lentivirus and AAV, rely on DNA template transfer to facilitate RNA delivery; Bioinspired vectors, including VLP, EV, and nanocages, utilize mechanisms like DNA template transfer, electroporation, and RNA-binding proteins; LNPs and PNPs achieve RNA delivery through electrostatic interactions and self-assembly properties to enhance cellular uptake; Other vectors, including MOF and QD, rely on electrostatic interactions to facilitate RNA binding and delivery.
Bioinspired vectors
Bioinspired vectors for RNA delivery are an innovative class of delivery systems that mimic biological entities such as viruses and cellular components to facilitate the efficient and targeted delivery of RNA molecules. These vectors leverage biological systems' natural design and functional characteristics, providing a promising approach to overcoming challenges associated with synthetic delivery systems. Bioinspired vectors encompass a variety of structures, including VLPs, nanocages, EVs, and exosomes [18, 79, 80]. VLPs are shell-like structures formed by engineered viral proteins that can encapsulate RNA, mimicking viral infection characteristics without the ability to replicate or cause disease. Nanocages are self-assembling protein sub-units ideal for encapsulating and protecting RNA molecules. EVs and exosomes are small vesicles naturally derived from cells that transport RNA and proteins through natural cellular pathways, facilitating targeted delivery and cellular uptake.
The progress in bioinspired vectors has been noteworthy in research and clinical contexts. VLPs have seen success in vaccine development, such as the hepatitis B vaccine, where they induce potent immune responses [81]. Exosomes are being explored for cancer therapy, utilizing their ability to specifically target tissues and evade the immune system [82]. Clinical trials are actively investigating the use of exosomes loaded with siRNA or miRNA to selectively alter gene expression in cancer cells [83], highlighting their potential in targeted cancer therapies.
The major benefits of bioinspired vectors include their high biocompatibility and low immunogenicity. Their natural or bioengineered origins generally make them more tolerable within the body, reducing the risk of adverse immune responses. Moreover, these vectors can leverage natural biological pathways for precise tissue targeting and efficient cellular uptake, crucial for minimizing off-target effects and maximizing therapeutic efficacy. Nevertheless, bioinspired vectors come with challenges, particularly in their production and purification, which can be complex and costly [84]. The variability in the composition and size of naturally derived vectors like EVs and exosomes also presents difficulties in achieving consistent results, complicating standardization and regulatory approval. Additionally, despite their natural origin, patient-specific immune responses can vary, introducing further challenges in their application.
Lipid nanoparticle vectors
LNPs are at the forefront of non-viral gene delivery systems, particularly noted for their success in the development of mRNA vaccines. Their unique structural and functional attributes allow for the efficient encapsulation and delivery of various nucleic acids. LNPs are typically composed of ionizable lipids that aid in encapsulating negatively charged nucleic acids, along with phospholipids, cholesterol, and polyethylene glycol (PEG)-modified lipids, which stabilize the NPs and extend their circulation time in the bloodstream [68, 69]. The ionizable lipids are crucial as they enable LNPs to respond to the acidic environment of endosomes following cellular uptake, facilitating the release of RNA into the cytoplasm.
The most notable success of LNP technology has been in mRNA vaccines, particularly for COVID-19. Beyond vaccines, LNPs are also being explored to deliver gene-editing tools like CRISPR-Cas9 and treat genetic diseases by delivering therapeutic mRNA or siRNA. For example, Onpattro, an LNP-formulated siRNA therapy, has been approved for treating hereditary transthyretin-mediated amyloidosis [85], showcasing the clinical viability of LNP-based therapies.
The most notable concerns of LNPs are the potential immunogenicity and inflammatory responses associated with the ionizable lipids and PEG components. Managing these responses is crucial for the safety and efficacy of LNP-based therapies. Additionally, producing LNPs requires sophisticated technology to ensure consistent quality and properties, which can be costly and technically demanding.
Polymer nanoparticle vectors
PNPs are a versatile class of carriers used for RNA delivery, made from biodegradable polymers that can encapsulate and protect RNA molecules while facilitating their entry into target cells. These NPs are gaining increasing attention for their potential in precision medicine, particularly in gene therapy and vaccine development. PNPs are typically made from synthetic polymers such as poly(lactic-co-glycolic acid) (PLGA), polyethylenimine (PEI), or natural polymers like chitosan [86, 87]. These materials are chosen for their biocompatibility and biodegradability, allowing the polymers to safely degrade into non-toxic byproducts that can be easily cleared from the body. Polymers can be engineered into various shapes and sizes and can be functionalized with targeting ligands or modified to respond to specific environmental triggers [88], such as pH changes, enhancing the release of RNA payloads into the target cytoplasm.
The study of PNPs for RNA delivery has significantly expanded, exploring their applications in gene silencing, mRNA-based vaccines, and CRISPR-Cas9 gene editing systems. In clinical settings, PNPs are being investigated in numerous trials, particularly in cancer treatment, where siRNA is used to silence oncogenes. For example, Calando Pharmaceuticals developed a PNP (CALAA-01) that delivers siRNA targeting the M2 subunit of ribonucleotide reductase, showing promising results in solid tumors [89]. In vaccines, PNPs are being explored for their ability to efficiently deliver mRNA vaccines, aiming to enhance immune responses while minimizing adverse effects.
The main advantages of PNPs include their protective and controlled release capabilities, which ensure that RNA therapies are effectively delivered and remain stable until they reach the target site [124]. Polymer modifiability allows for precise tuning of NP properties, such as degradation rate, mechanical strength, and interactions with biological barriers, making them highly adaptable to various therapeutic needs. Additionally, by attaching specific ligands to their surface, PNPs can be designed to target specific tissues or cell types, enhancing the specificity and potency of RNA delivery.
However, challenges associated with PNP vectors also exist [90]. A primary concern is the potential cytotoxicity, particularly when using cationic polymers like PEI, which may disrupt cell membranes and lead to inflammatory responses. Additionally, the variability in the synthesis of PNPs can lead to batch-to-batch inconsistencies, posing scalability and clinical application challenges. Designing polymers that degrade at an appropriate rate to effectively release their payloads without premature degradation or prolonged retention in the body is another significant technical hurdle.
Other vectors
In addition to the more commonly used lipid and PNPs, other NP vectors for RNA delivery include a diverse range of materials such as MOFs, QDs, and silica-based NPs. These carriers offer unique properties that can enhance the delivery, stability, and targeting of RNA therapies, making them valuable tools in advancing gene therapy.
As exemplified by ZIF-8, MOFs are crystalline frameworks composed of metal ions and organic ligands, offering large surface areas and customizable porosity for effective RNA encapsulation [91]. QDs, primarily recognized for their fluorescent properties, are now being adapted for RNA delivery [92], providing the dual benefit of therapeutic delivery and real-time imaging. Silica-based NPs, especially mesoporous variants, are valued for their large surface areas and chemical stability, which are ideal for RNA loading and controlled release [93]. Preclinical studies have demonstrated the potential of these vectors. For instance, ZIF-8 MOFs have shown promise in RNA protection and gene silencing in cancer models. QDs are being explored to track RNA therapies while delivering therapeutic payloads. Silica-based NPs have effectively delivered siRNA for lung cancer, improving RNA stability and targeted release. While MOFs, QDs, and silica NPs are still in the experimental phase, their unique capabilities present exciting possibilities for RNA delivery in gene therapy. Continued research and development will be crucial in addressing their limitations and unlocking their full potential in clinical applications.
Various vector types are employed to enhance the delivery, stability, and specificity of gene therapies. Each vector type offers distinct advantages and faces unique challenges, making the choice of vector crucial for the success of therapeutic applications. Table 1 provides a comparative overview of different vectors used in gene delivery, highlighting their key features, benefits, and limitations. This comparison aims to guide the selection of appropriate delivery systems for RNA-based therapies in HCC and other diseases.
Comparison of different types of vectors for RNA delivery
| Vector type | Examples | Advantages | Challenges | Applications |
|---|---|---|---|---|
| Viral Vectors | AAV, lentivirus, adenovirus | High transduction efficiency, sustained gene expression | Immunogenicity, risk of insertional mutagenesis, complex and costly production | Gene therapy (e.g., Luxturna™, Zolgensma™) |
| Bioinspired Vectors | VLPs, Nanocages, Exosomes, EVs | High biocompatibility, reduced immunogenicity, natural targeting mechanisms | Complex production and purification, variability in composition | Cancer therapy, targeted RNA delivery |
| Lipid Nanoparticles | Commonly used for mRNA and siRNA delivery | High biocompatibility, enhances cellular uptake, protects RNA from degradation | Potential immunogenicity, requires sophisticated manufacturing | mRNA vaccines (e.g., COVID-19 vaccines), gene therapy |
| Polymer Nanoparticles | PLGA, PEI-based NPs | Biocompatible, customizable surface chemistry for targeted delivery | Potential cytotoxicity, variability in synthesis leading to inconsistent results | siRNA delivery, cancer therapy |
| Other vectors | MOFs, QDs, Mesoporous silica NPs | high surface area, tunable porosity, pH-responsive release | Biodegradability concerns, potential metal ion toxicity | Gene silencing in cancer models |
Characteristics of the liver and HCC
Before delving into the innovative realm of RNA nanomedicine for liver cancer therapy, it is crucial to comprehensively elucidate the structural and functional characteristics of the liver and HCC. This section examines the liver's unique anatomical structure and functional attributes, detailing its pivotal roles in metabolism, detoxification, and immune regulation, all essential for optimizing RNA nanotherapeutic strategies. Additionally, it explores the specific pathophysiological features of liver cancer, particularly HCC, including the TME and molecular heterogeneity that influence the efficacy of therapeutic interventions. Understanding these characteristics is fundamental to the development of RNA nanomedicines that can effectively target and treat liver cancer, providing a theoretical foundation for enhancing therapeutic efficiency and precision.
Liver structure and function
As the largest visceral organ, the liver plays a crucial role in numerous physiological processes vital for survival and health. Beyond its metabolic functions, the liver supports immune responses by eliminating pathogens and exogenous antigens, underscoring its status as the body's largest metabolic organ [94]. Its complex structural and functional framework is key to the development of targeted RNA nanotherapeutics. The liver's extensive vascular network, with dual blood supply from the hepatic artery and portal vein, not only facilitates nutrient and drug delivery but also significantly influences the distribution and metabolism of therapeutic agents, including RNA nanotherapeutics [95]. The liver's anatomical complexity, with lobules containing hepatocytes and non-parenchymal cells such as Kupffer cells, hepatic stellate cells, and liver sinusoidal endothelial cells (LSECs), is central to understanding targeted RNA delivery. Hepatocytes are involved in metabolism and protein synthesis, while LSECs and Kupffer cells modulate immune and endocytic functions, offering specific targets for RNA therapies [96-99]. These extensive functional capacities are highly relevant to RNA therapies, which often aim to modulate specific metabolic pathways associated with diseases like HCC.
Given the liver's filtering capacity and complex microenvironment, designing RNA nanomedicines requires specific adaptations to enhance delivery efficiency. For instance, leveraging the high endocytic activity of LSECs can enhance the efficiency of RNA delivery systems, and specific cellular interactions within the liver microenvironment can be exploited to improve the uptake and efficacy of therapeutic RNA [100]. Recent studies have shown that after entering the liver, PEGylated liposomal drugs are first taken up by Kupffer cells, where the liposomes are degraded intracellularly, releasing free drugs that evade LSEC capture and directly enter hepatocytes [101]. The amount of liposomal drug captured by Kupffer cells positively correlates with subsequent drug accumulation in hepatocytes. These highlight the importance of understanding liver-specific uptake mechanisms to optimize nanoparticle formulations for HCC. Advanced strategies for targeted delivery in the liver aim to improve stability, enhance tumor specificity, and avoid rapid metabolism or clearance, thus maximizing therapeutic efficacy and minimizing side effects [102, 103].
Structural and microenvironmental features of HCC
The TME of HCC is highly complex and plays a central role in disease progression and therapy response. HCC often exhibits diverse morphological features, ranging from well-differentiated to poorly differentiated, due to intratumoral heterogeneity [104]. This variability contributes to its aggressive behavior and challenges therapeutic efficacy, as tumor regions differ in vascularization and cellular composition [105, 106]. Unlike the finely organized vasculature of normal liver tissue, HCC often exhibits disorganized and unstructured vascularization. This abnormal vasculature leads to hypoxic conditions within the tumor, driving further genetic instability and tumor progression [107, 108]. Arteriovenous shunting and sinusoidal endothelial cell capillarization are typical findings in HCC [109], complicating drug delivery.
Moreover, the TME of HCC comprises various cell types, including immune cells (T cells, macrophages), fibroblasts, and endothelial cells, along with the extracellular matrix (ECM) [110]. These components interact dynamically, creating either pro-tumor or anti-tumor conditions. Chronic inflammation in HCC, caused by precursor conditions like hepatitis or cirrhosis, fosters an immunosuppressive TME, making effective treatment challenging [111]. For example, Regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and cancer-associated fibroblasts (CAFs) all play roles in promoting immune evasion and tumor progression [112-114].
Understanding the dynamics of the HCC TME is crucial for designing effective RNA-based therapies. By targeting specific components of the TME, RNA nanotherapeuitcs can modulate immune suppression, promote immune activation, and inhibit critical pathways involved in tumor progression [115]. RNA nanotherapeutics can be designed to silence genes critical for tumor cell survival and proliferation or to modulate the immune environment, enhancing the presentation of tumor antigens and restoring the activity of effector immune cells to improve therapeutic outcomes [116]. This comprehensive understanding of liver and TME features allows for the development of targeted strategies that leverage tumor vulnerabilities for more effective treatment outcomes.
Strategies for targeted delivery in HCC
The effective delivery of RNA nanotherapeutics for HCC necessitates a thorough understanding of the liver's unique anatomy, physiological characteristics, and the complex TME specific to HCC. To enhance specificity while minimizing off-target effects and systemic toxicity, advanced delivery strategies have been developed. The following subsections provide an in-depth exploration of these approaches, each designed to address the unique challenges and take advantage of the liver's and HCC's microenvironmental characteristics.
Utilizing HCC-specific receptors for improved tumor selectivity
Targeting hepatocellular carcinoma-specific receptors is a critical strategy for enhancing the selectivity of RNA nanomedicine delivery, thereby improving treatment efficacy while minimizing side effects. GPC3 is a highly promising target for HCC-specific delivery, as it is overexpressed on HCC cells but largely absent in normal liver tissue [117]. Antibody-functionalized nanoparticles, such as those modified with anti-GPC3 antibodies, have demonstrated significant efficacy in delivering RNA molecules directly to HCC cells, allowing for targeted silencing of oncogenic pathways or activation of tumor suppressor genes. Preclinical studies have shown that such nanoparticles can selectively accumulate in GPC3-positive tumors, reducing the risk of off-target effects in healthy liver tissues.
Asialoglycoprotein receptor (ASGPR) is another critical target for enhancing selectivity. ASGPR is predominantly expressed on hepatocytes, and leveraging ligands such as N-acetylgalactosamine (GalNAc) enables efficient receptor-mediated endocytosis of nanoparticles carrying RNA payloads. This receptor is already being utilized successfully in clinical settings, such as in Inclisiran, an siRNA therapeutic targeting cholesterol synthesis via hepatic ASGPR uptake. This approach demonstrates the potential for GalNAc-functionalized nanoparticles in delivering RNA therapeutics specifically to the liver, effectively bypassing non-hepatic tissues [118]. Similarly, the transferrin receptor, which is overexpressed in many cancers including HCC, has been utilized to improve nanoparticle uptake by tumor cells. Transferrin-functionalized nanoparticles carrying siRNA or miRNA have shown increased selectivity and uptake by HCC cells, as HCC tends to have a higher demand for iron compared to healthy cells [119]. This not only enhances the efficacy of the therapeutic RNA but also reduces the likelihood of systemic side effects, making transferrin a valuable ligand in targeted nanoparticle design [120]. Folate receptors (FR) and epidermal growth factor receptor (EGFR) are also promising targets for HCC-specific delivery [121]. While folate receptors are expressed in more aggressive HCC subtypes, EGFR is frequently upregulated in HCC, particularly in poorly differentiated tumors. Anti-EGFR-modified nanoparticles and folate-functionalized carriers have been effectively utilized to deliver siRNA or mRNA to suppress tumor growth, demonstrating improved outcomes in HCC models.
Leveraging liver fenestrations for enhanced nanoparticle delivery
The fenestrated architecture of LSECs offers a unique avenue for enhancing nanoparticle delivery [122]. LSECs contain fenestrations, transcellular pores approximately 50-150 nm in size, that facilitate the movement of substances, including nanoparticles, from the bloodstream into the liver parenchyma. This fenestrated structure allows for the passive accumulation of nanoparticles in the liver, provided they are appropriately designed in terms of size and surface characteristics. Optimizing the size of nanoparticles to match the dimensions of LSEC fenestrations allows for effective translocation to hepatocytes or HCC cells. LNPs and PNPs, when sized appropriately (generally below 100 nm), can readily traverse LSEC fenestrations and accumulate in hepatic tissues [123]. Recent advancements in size-tunable polymeric micelles have demonstrated improved delivery to the liver by adjusting nanoparticle size to optimally pass through the fenestration [124]. Such size optimization is critical to ensuring enhanced hepatic accumulation while minimizing non-specific distribution in other organs.
Overcoming the TME barriers for efficient delivery
The TME of HCC poses significant challenges for effective therapeutic delivery, characterized by a dense ECM, abnormal vasculature, and hypoxic regions [125]. To overcome these barriers, advanced strategies are being employed to enhance the efficacy of RNA nanomedicines. The enhanced permeability and retention (EPR) effect, resulting from leaky vasculature in tumors, facilitates the passive accumulation of nanoparticles in the tumor tissue, which provides a foundational mechanism for RNA-based nanomedicines.
Beyond passive targeting, pH-sensitive and hypoxia-responsive nanoparticles have been developed to enhance delivery under specific TME conditions [126]. These nanoparticles are stable during circulation but are designed to release their RNA payload under the acidic or hypoxic conditions found within HCC tumors. To address the challenge of dense ECM, nanoparticles can be functionalized with hyaluronidase, which degrades the ECM components, thereby enhancing nanoparticle penetration and uniform distribution throughout the tumor. This enzyme-functionalization approach enables nanoparticles to reach poorly vascularized regions within the tumor, ensuring more comprehensive coverage and efficacy.
Furthermore, Kupffer cells and LSECs, which play key roles in nanoparticle uptake and biodistribution. Kupffer cells, the resident macrophages of the liver, are responsible for filtering out foreign particles from the blood. PEGylated liposomes, for example, are taken up by Kupffer cells, where they are subsequently degraded to release the active RNA payloads, which may then reach hepatocytes and tumor cells [101]. This sequential process allows for efficient accumulation of therapeutic agents within hepatic tissues. In addition, LSECs possess high endocytic activity, which can be leveraged to facilitate RNA nanoparticle uptake [127]. Functionalizing nanoparticles with positively charged peptides or cationic lipids enhances their interaction with LSECs, leading to improved internalization and delivery to HCC cells or hepatocytes. By optimizing these cell-specific interactions, nanoparticles can achieve more efficient hepatic and tumor-specific delivery.
Enhancing biocompatibility and minimizing off-target effects
Biocompatibility and minimizing immune responses are crucial for the success of RNA-based therapies in HCC. Biomimetic carriers, such as EV-like particles or cell membrane-coated nanoparticles, are increasingly being utilized to enhance biocompatibility. These biomimetic nanoparticles exhibit reduced immunogenicity due to their natural origin, allowing them to evade immune recognition and prolong systemic circulation, which is essential for successful repeated administration. Also, the biomimetic carriers could be further engineered with HCC targeting ligand to enhance the HCC targeting efficacy, such as our team reported that transferrin displayed 293T cell membrane-coated EV and NGR peptide expressed red blood cell membrane-coated EV exhibited much higher HCC accumulation than the non-engineered EV [128, 129].
In addition to biomimetic strategies, stimuli-responsive nanoparticles have been developed that release their RNA payload only upon exposure to specific conditions found in the TME, such as an acidic pH or the presence of enzymes like matrix metalloproteinases (MMPs) [130]. This specificity allows for the precise targeting of HCC cells while minimizing damage to normal liver cells. MMP-responsive nanoparticles carrying siRNA or mRNA targeting tumor growth factors have shown efficacy in preclinical HCC models by releasing their cargo in the presence of elevated MMPs, a characteristic feature of the HCC TME.
The unique anatomical and physiological features of the liver, coupled with the complex TME in HCC, present challenges and opportunities for targeted delivery of RNA-based nanomedicines. By focusing on HCC-specific receptors for tumor selectivity, utilizing liver fenestrations for effective nanoparticle translocation, overcoming TME barriers through advanced nanoparticle designs, leveraging specialized liver cell functions, and enhancing biocompatibility, RNA nanotherapeutics hold significant promise for precise and effective HCC treatment. These strategies represent major advancements over traditional therapeutic approaches, providing targeted, safe, and efficient treatment options for HCC patients.
Applications of RNA nanotherapeutics for HCC treatment
RNA nanotherapeutics offer a promising approach for treating HCC, leveraging advanced NP delivery systems to target and regulate key genetic pathways associated with cancer progression. These therapies include siRNA for gene silencing, miRNA modulation, and mRNA and saRNA for protein expression, all delivered through NPs designed to enhance stability, cellular uptake, and targeted delivery to HCC cells. By utilizing these technologies, RNA nanotherapeutics aim to overcome the limitations of traditional treatments, offering more precise, effective, and personalized treatment options for HCC patients.
Gene regulation via miRNA nanotherapeutics
miRNA nanotherapeutics represents a sophisticated and emerging approach for treating HCC. miRNA nanotherapeutics based therapies aim to restore normal gene expression patterns in HCC, thereby inhibiting tumor growth and progression. In HCC, specific miRNAs can function as either tumor suppressors or oncogenes. Over the past decade, significant progress in miRNA nanotherapeutics for HCC has been made, thanks to deeper insights into miRNA biology and advancements in delivery technologies.
One key example is miR-141, a tumor suppressor whose expression is often downregulated in HCC, leading to uncontrolled growth and metastasis [131, 132]. Restoring miR-141 levels using a tumor-adhesive NPX-glue nanoparticle system effectively inhibits tumor growth by ensuring localized delivery at the tumor site, maximizing its therapeutic potential while minimizing side effects [133]. Similarly, miR-122, a liver-specific miRNA often downregulated in HCC, is one of the most prevalent gene in HCC. The loss of miR-122 is linked to enhanced tumor growth, metastasis, and poor prognosis [134]. Researchers have developed NP-based delivery systems to restore miR-122 levels in HCC models. For instance, LNPs encapsulating miR-122 mimics have effectively restored miR-122 levels in liver tumors, suppressing the expression of oncogenes like Cyclin G1 and ultimately reducing tumor growth and metastasis [135].
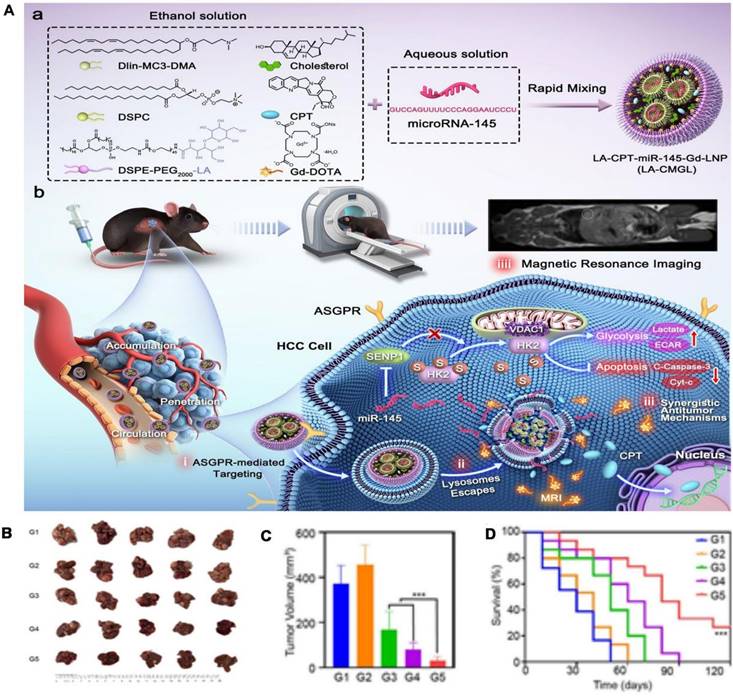
Another crucial miRNA is miR-145, which acts as a tumor suppressor by inhibiting pathways involved in cell proliferation and metastasis. As shown in Figure 4, the study utilizes a lipid nanoparticle system, LA-CPT-miR-145-Gd-LNP (LA-CMGL), co-loaded with camptothecin (CPT) and miR-145, designed for targeted delivery to HCC cells [136]. The nanoparticles are modified with lactobionic acid (LA) to target ASGPR overexpressed on HCC cells, enhancing cellular uptake through ASGPR-mediated endocytosis. Upon delivery, miR-145 exerts its tumor-suppressive effects by inhibiting oncogenic pathways, while CPT induces apoptosis, resulting in a synergistic antitumor effect. Additionally, Gd-DOTA provides MRI visibility, allowing for real-time monitoring of nanoparticle accumulation in tumors. This theranostic approach demonstrates significant tumor growth suppression and extended survival in HCC models, highlighting the potential of miR-145 in combination with chemotherapy for effective HCC therapy. These preclinical successes have spurred interest in clinical trials for miR-122-based therapies.
The clinical translation of miRNA nanotherapeutics is gaining momentum, with several candidates entering early-stage clinical trials. A notable example is MRX34, a liposomal formulation of miR-34a mimic, targeting multiple oncogenes involved in HCC progression, including MYC and BCL-2. MRX34 was the first miRNA mimic to enter clinical trials for cancer treatment [137]. Although early trials showed anti-tumor activity in patients with advanced HCC and other solid tumors, the trial was halted due to immune-related adverse events, highlighting the challenges of miRNA therapy and the need for further optimization of delivery systems and dosing regimens. Another promising candidate is miR-26a, which is downregulated in HCC. Restoring miR-26a through nanoparticle-based delivery, such as exosomes, has shown efficacy in reducing tumor burden by targeting Cyclin D2 and E2 [138, 139].
Recent advancements in nanoparticle (NP) technology are further improving miRNA delivery. pH-sensitive NPs that release their payload in the acidic tumor environment, NPs that selectively bind to receptors overexpressed on HCC cells, and hybrid NPs combining multiple delivery strategies are all being developed to enhance specificity, stability, and therapeutic efficacy [140].
miRNA nanotherapeutics offer significant advantages over traditional therapies by regulating multiple genes simultaneously, thus addressing the complexity of HCC biology [141]. NP delivery systems enhance the stability and bioavailability of miRNAs, ensuring their effective delivery to tumor sites while minimizing off-target effects. Additionally, miRNA therapy can be customized based on the individual patient's characteristics, providing a more effective and less toxic personalized treatment strategy.
Overall, miRNA nanotherapeutics illustrate a promising and innovative approach for treating HCC by leveraging the regulatory potential of miRNAs to modulate gene expression and inhibit tumor growth. Through the use of advanced NP delivery systems, these therapies offer enhanced stability, targeting, and efficacy, addressing key challenges in HCC treatment. As research progresses and clinical trials continue, miRNA-based therapies have the potential to become a critical component of HCC management, offering new hope for effective and personalized cancer treatment.
Gene silencing via siRNA nanotherapeutics
Gene silencing via RNA nanotherapeutics exhibit a cutting-edge approach for treating HCC, utilizing siRNA to target and silence specific oncogenes involved in cancer progression. These therapeutic agents are delivered through advanced NP systems that enhance siRNA stability in the bloodstream, facilitate cellular uptake, and ensure targeted delivery to HCC cells, thereby improving therapeutic outcomes. In HCC, oncogenes such as MYC, VEGF, and BCL-2 are often overexpressed, promoting uncontrolled cell proliferation, angiogenesis, and resistance to apoptosis [142, 143]. By designing siRNA molecules that specifically target these oncogenes, RNA nanotherapy can effectively reduce the expression of these harmful proteins, thereby inhibiting tumor growth and progression.
Preclinical studies have demonstrated the promise of siRNA-mediated gene silencing in HCC. siRNA targeting VEGF has been shown to inhibit angiogenesis, thereby reducing the tumor's blood supply and slowing disease progression [144]. Similarly, siRNA targeting MYC has significantly reduced tumor cell proliferation and induced apoptosis [145]. Clinical trials are currently exploring the efficacy of siRNA therapies in HCC, with several NP-based siRNA formulations under investigation. ALN-VSP, an LNP composed of kinesin spindle protein (KSP) siRNA and VEGF siRNA in a 1:1 ratio, was well tolerated and prolonged disease stabilization in participants with nodal and extensive liver metastasis [146]. These trials aim to evaluate the therapeutic effectiveness, safety, and potential side effects of these novel therapies.
Several siRNA nanotherapeutics based therapies have been designed to target specific oncogenes in HCC. For instance, siRNA targeting BCL-2, a gene that inhibits apoptosis, has shown to sensitize HCC cells to chemotherapy by promoting cell death [147]. Another notable example is siRNA targeting β-catenin, a key player in the Wnt signaling pathway [148], which is crucial for HCC development and progression. By silencing β-catenin, researchers have observed reduced tumor growth and increased sensitivity to other therapeutic agents. These examples highlight the potential of siRNA therapy to disrupt critical oncogenic pathways in HCC, offering a targeted treatment approach.
miRNA nanotherapeutics achieved HCC treatment. (A) Schematic and experimental validation of the LA-CPT-miR-145-Gd-LNP (LA-CMGL) system for targeted, MRI-visible therapy in HCC, and mechanism of ASGPR-mediated targeting, cellular uptake, lysosomal escape, and synergistic antitumor effects in HCC cells, alongside MRI imaging capability for tracking accumulation. (B) Representative images of tumor samples across treatment groups. (C) Tumor volume comparison indicating enhanced efficacy of LA-CMGL. (D) Survival analysis showing improved outcomes in treated groups compared to controls. Adapted from [136]. Copyright 2024, Springer Nature.
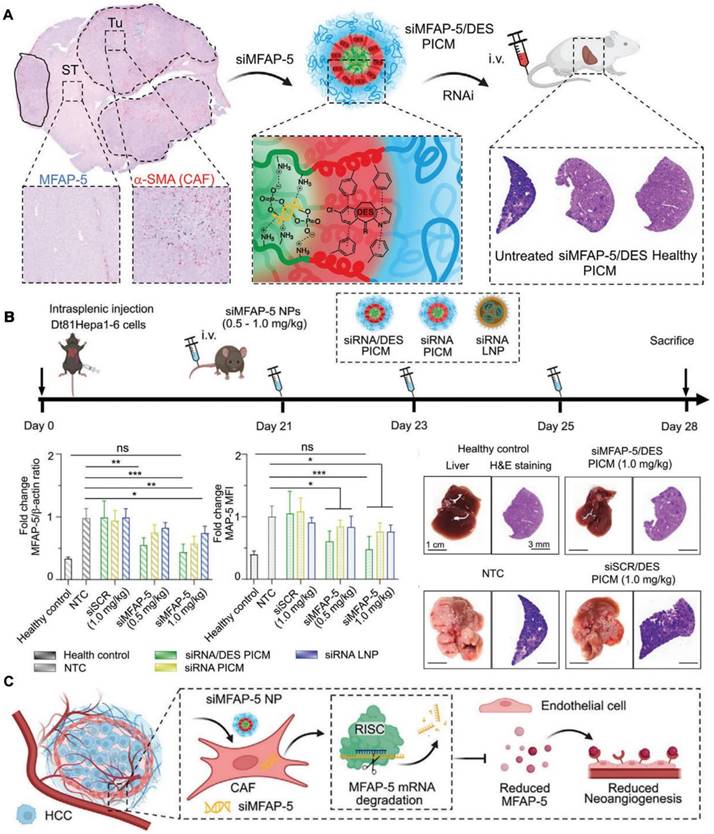
Beyond directly targeting HCC cells, siRNA nanotherapy also addresses the TME, particularly cancer-associated fibroblasts (CAFs). CAFs significantly contribute to tumor progression and angiogenesis, making them crucial therapeutic targets. Recent research highlights the development of polyion complex micelles (PICMs) based on triblock polypept(o)ides, which serve as an efficient delivery system for siRNA specifically targeting microfibrillar-associated protein 5 (MFAP-5) (Figure 5) [149]. This protein is essential in the TME, contributing to tumor growth by enhancing angiogenesis. By co-encapsulating siRNA with cationic amphiphilic drugs (CADs) like desloratadine (DES), these micelles improve endosomal escape and gene silencing efficiency, leading to significant tumor burden reduction in HCC models. This approach not only directly affects cancer cells but also disrupts the supportive TME, providing a promising strategy for HCC treatment.
The strategy of siMFAP-5/DES PICMs in disrupting the tumor-supportive environment by targeting CAFs to treat HCC. (A) Schematic illustration of the siMFAP-5/DES PICM design and mechanism. The figure shows the encapsulation of siMFAP-5 in the DES PICM, which targets CAFs identified by α-SMA staining in HCC tissues. The siMFAP-5/DES PICMs are administered intravenously, leading to RNAi that specifically silences the MFAP-5 gene in CAFs within the TME. (B) In vivo treatment timeline and therapeutic outcomes in a murine HCC model. Mice injected with Dt81Hepa1-6 cells were treated with siMFAP-5 PICMs, showing a significant reduction in MFAP-5 expression in CAFs, with comparative analyses of siRNA PICMs, siRNA LNPs, and control treatments. (C) The mechanism is that siMFAP-5 PICMs specifically target and degrade MFAP-5 mRNA in CAFs via RISC, leading to reduced angiogenesis and tumor progression in HCC. Adapted from [149]. Copyright 2024, Wiley.
The primary advantage of siRNA nanotherapeutics depend on its specificity. Unlike traditional chemotherapy, which can affect both cancerous and healthy cells, siRNA specifically targets oncogenes, minimizing off-target effects and reducing toxicity. Additionally, the use of NP delivery systems enhances siRNA stability and bioavailability, allowing for more effective delivery to tumor sites. This targeted approach also provides the potential for combination therapies, where siRNA can be used alongside other treatments to enhance overall efficacy and overcome resistance mechanisms in HCC. Recent advancements also include exploring multi-target siRNA strategies, where a single NP can deliver siRNAs targeting multiple oncogenes [150]. This approach is particularly relevant in HCC, which is driven by various genetic and epigenetic alterations. By silencing multiple pathways simultaneously, researchers aim to achieve more comprehensive tumor control and reduce the likelihood of resistance development.
Gene silencing via RNA nanotherapy is an innovative and promising approach for treating HCC, leveraging the precision of siRNA to target and silence specific oncogenes involved in cancer progression. Through the use of advanced NP delivery systems, these therapies offer improved stability, targeting, and therapeutic efficacy, addressing key challenges in HCC treatment. As research continues and clinical trials progress, siRNA-based therapies have the potential to become a cornerstone of HCC management, providing patients with more effective and less toxic treatment options.
mRNA nanotherapeutics for protein restoration in HCC
mRNA nanotherapeutics represent an innovative approach for treating HCC by directly restoring protein function through the delivery of synthetic mRNA molecules. Unlike traditional therapies that rely on small molecules or antibodies to inhibit protein activity, mRNA therapy aims to reintroduce or enhance the expression of therapeutic proteins that are missing or dysfunctional in cancer cells. These synthetic mRNAs are encapsulated in NPs, typically LNPs, which protect the mRNA from degradation, facilitate cellular uptake, and ensure effective delivery to target tissues [151]. Once delivered to cells, the encapsulated mRNA is translated by the host's ribosomes into the corresponding protein, effectively restoring or enhancing the function of critical proteins that control cell growth, apoptosis, and immune responses. This approach is particularly beneficial in HCC, where certain tumor suppressor genes or regulatory proteins may be downregulated or inactivated due to genetic mutations or epigenetic modifications.
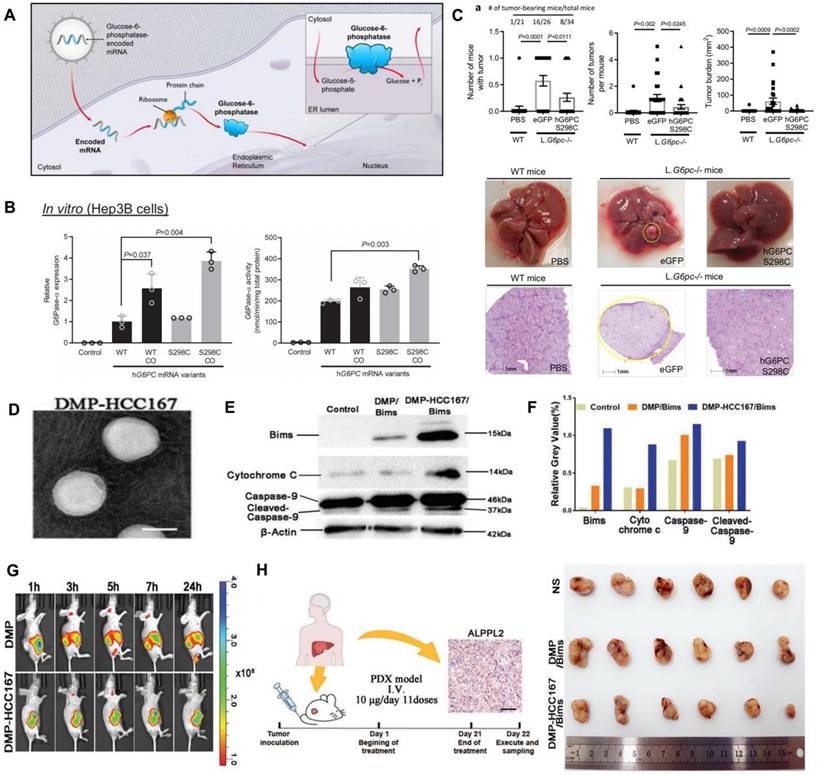
Research on mRNA nanotherapeutics for HCC has shown promising progress in preclinical models. For example, restoring the expression of tumor suppressor proteins like p53, which is often mutated or downregulated in HCC, has been a key focus. Delivering mRNA encoding functional p53 using LNPs has led to significant inhibition of tumor growth and induction of apoptosis in HCC cells in experimental models [152]. Another area of focus is the delivery of mRNA-encoding cytokines and immunoregulatory proteins to enhance anti-tumor immune responses in HCC. For example, mRNA encoding IL-12 has been studied for its potential to stimulate immune cells to more effectively attack HCC tumors [153, 154]. Preclinical studies have shown that IL-12 mRNA delivered via NPs can enhance immune cell infiltration into tumors, leading to improved tumor control and, in some cases, complete regression of established tumors. Therefore, IL-12 mRNA is used to stimulate the immune system to target and destroy cancer cells. Delivering IL-12 mRNA directly to tumor cells via NPs, the therapy can induce local production of IL-12 within the TME. This localized production of IL-12 enhances the immune surveillance by recruiting and activating cytotoxic T cells and NK cells to the tumor site. Additionally, metabolic dysregulation is a critical factor in the development and progression of HCC, as altered glucose and lipid metabolism provide the energy and building blocks necessary for rapid tumor growth. In particular, deficiencies in enzymes like glucose-6-phosphatase-α (G6Pase-α), which regulates glucose production in the liver, create a metabolic environment conducive to HCC. Targeting and correcting metabolic pathways offer a promising strategy for HCC treatment. As shown in Figure 6A-C, the study investigates the therapeutic potential of delivering G6Pase-α mRNA to restore glucose metabolism in glycogen storage disease type 1a (GSD1a), a condition characterized by G6Pase-α deficiency and a high risk of HCC [155]. By delivering G6Pase-α mRNA in LNPs, the treatment aims to normalize glucose production, reduce glycogen buildup, and mitigate tumor development. The findings demonstrate effective mRNA expression, increased enzyme activity, and a reduction in liver tumor incidence in GSD1a mouse models, highlighting mRNA therapy as a potential metabolic treatment for preventing HCC.
Although mRNA delivery for HCC shows great potential, the precision of delivery to HCC cells remains a critical challenge, limiting therapeutic outcomes. To address this, a study on 1,2-dioleoyl-3-trimethylammonium-propane (DOTAP)-methoxy poly(ethylene glycol) (mPEG)-poly(ε-caprolactone) (PCL) linked HCC167 peptide (DMP-HCC167) focuses on the development of a highly specific delivery system for mRNA-based therapy targeting HCC [156]. DMP-HCC167 is a phage display-derived peptide that exhibits a strong affinity for the ALPPL2 receptor, which is overexpressed in HCC cells. By conjugating this peptide to LNPs, the researchers engineered a delivery system that can precisely target and deliver therapeutic mRNA to HCC cells, thereby enhancing the therapeutic efficacy. The specificity of DMP-HCC167 for HCC cells was demonstrated through a series of experiments, showing its superior targeting capabilities compared to non-specific delivery methods (Figure 6D-H). This specific delivery is crucial as it ensures that the therapeutic mRNA is predominantly taken up by HCC cells, thereby reducing off-target effects and enhancing the treatment's overall effectiveness. The study underscores the importance of developing targeted delivery systems like DMP-HCC167 to improve the outcomes of mRNA therapies in treating HCC.
mRNA nanotherapeutics for HCC treatment. (A) Schematic and experimental validation of G6PC mRNA therapy for glucose-6-phosphatase deficiency, shows the mechanism of G6Pase-α mRNA delivery and expression, enabling glucose production in hepatocytes. (B) Validation of G6Pase-α mRNA expression and activity in Hep3B cells. (C) Tumor development in L.G6pc-/- mice treated with wild-type or mutant G6PC mRNA, with representative liver tumor images and histological examination in treated mice. Adapted from [155]. Copyright 2021, Springer Nature. (D) TEM image of DMP-HCC167 NPs, designed for targeted delivery to HCC. (E) WB analysis shows the expression of apoptosis-related proteins in HCC cells treated with DMP-HCC167, indicating effective induction of apoptosis. (F) Quantification of WB. (G) Biodistribution study showing targeted delivery of DMP-HCC167 NPs to tumor sites in a PDX model of HCC over time, as observed via live imaging. (H) DMP-HCC167 NPs significantly reduced tumor size compared to control treatments in a PDX model of HCC. Adapted from [156]. Copyright 2022, Wiley.
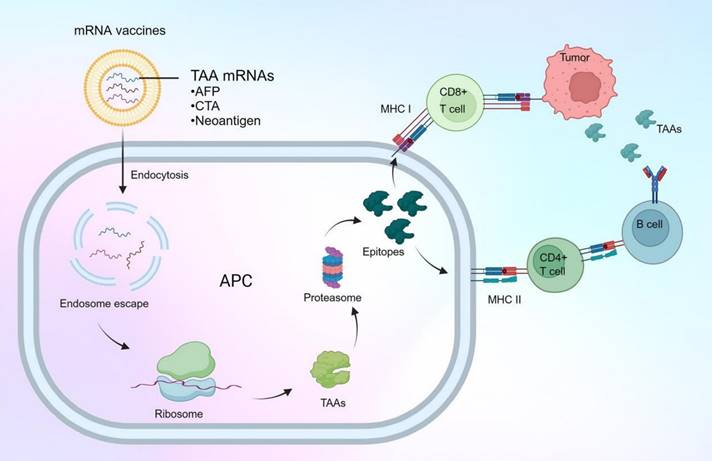
Additionally, mRNA nanotherapy is making significant strides in vaccine development for HCC, representing a breakthrough in cancer immunotherapy. These vaccines are designed to stimulate the patient's immune system to recognize and attack cancer cells, providing a highly targeted approach to combating HCC [13, 157, 158]. As shown in Figure 7, unlike traditional vaccines that often use inactivated viruses or proteins, mRNA vaccines utilize synthetic mRNA to encode tumor-associated antigens (TAAs) or neoantigens specific to a patient's tumor. To ensure effective delivery and uptake by immune cells, particularly dendritic cells, these mRNA molecules are encapsulated in LNPs. In HCC, mRNA vaccine development has focused on targeting specific TAAs such as alpha-fetoprotein (AFP) and GPC3 [159], which are often overexpressed in liver cancer cells. By targeting these antigens, mRNA vaccines can help direct the immune system to selectively attack HCC cells while sparing normal liver tissue.
In addition to targeting known TAAs, researchers are also exploring the use of personalized mRNA vaccines targeting neoantigens, which are generated by tumor-specific mutations. This approach is particularly promising in HCC, which often exhibits high genetic heterogeneity. By sequencing a patient's tumor and identifying neoantigens, researchers can create personalized mRNA vaccines that target the unique mutation profile of the tumor, potentially leading to more effective and durable immune responses.
mRNA vaccines for HCC treatment offer several notable advantages [160]. First, mRNA vaccines are non-infectious and non-integrative, eliminating the risk of insertional mutagenesis and other genetic alterations. They are also highly adaptable, allowing for rapid design and production in response to emerging tumor antigens or changes in a patient's tumor profile. This adaptability is particularly valuable in personalized medicine, where treatments can be tailored to the specific needs of the patient.
mRNA nanotherapeutics provide a promising approach for HCC treatment through protein restoration and vaccine development. By encapsulating mRNA in LNPs, therapeutic proteins such as tumor suppressors are directly delivered to HCC cells, helping to inhibit tumor growth and enhance treatment efficacy. As vaccines, mRNA nanotherapeutics encode tumor-associated antigens, stimulating the immune system to target and destroy cancer cells. These strategies have shown significant potential in preclinical and early clinical trials, offering new targeted and adaptable treatment options for HCC.
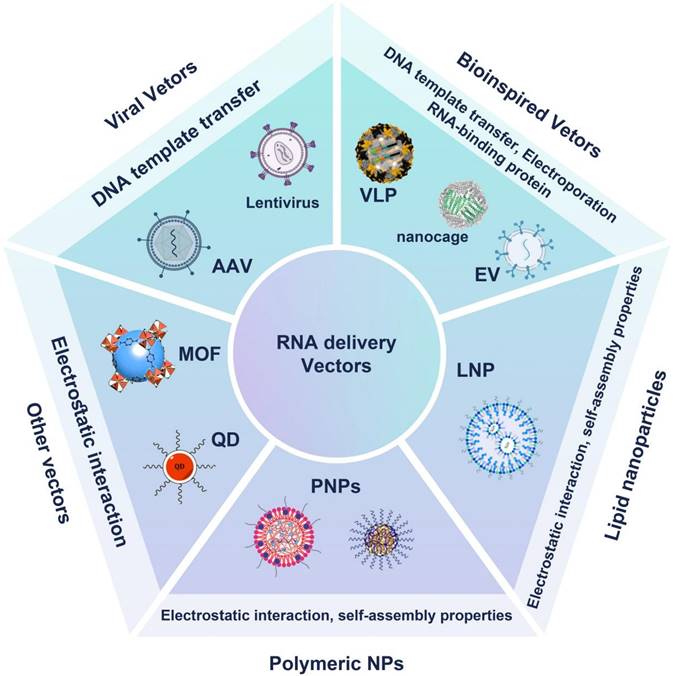
The development of mRNA HCC vaccine encoding tumor-associated antigens or neoantigens. The mRNA vaccines, which encode TAAs such as AFP, CTA, and neoantigens, are delivered into antigen-presenting cells (APCs) through endocytosis. Following endosome escape, the mRNA is translated by ribosomes into TAA proteins within the APC. These TAAs are then processed by the proteasome into smaller peptide fragments (epitopes). The epitopes are presented on the cell surface by major histocompatibility complex (MHC) molecules: MHC I presents them to CD8+ T cells, leading to cytotoxic T cell activation and tumor cell apoptosis, while MHC II presents them to CD4+ T cells, aiding in B cell activation and antibody production. This process initiates an adaptive immune response specifically targeting tumor cells expressing the TAAs. Created with BioRender.com.
saRNA nanotherapeutics for HCC via protein expression enhancement
saRNA nanotherapeutics represent a novel approach to HCC treatment by enhancing the expression of beneficial genes rather than silencing them like siRNA. This mechanism, known as RNA activation (RNAa), differs from the gene-silencing effect of siRNA, allowing for the reactivation of tumor suppressor genes or other therapeutic genes that are downregulated in cancer cells. When delivered using advanced NP systems such as LNPs or PNPs, saRNAs can be effectively transported to target cells, where they bind to the promoter regions of specific genes [161]. This binding recruits transcription factors, leading to increased transcription and expression of the target gene. In HCC, the downregulation of tumor suppressors and other regulatory genes is common, and saRNA therapy offers the potential to restore normal cellular function and inhibit tumor progression [162].
The development of saRNA nanotherapeutics for HCC is an emerging field, with significant progress made in preclinical studies. One key target for saRNA therapy in HCC is the E-cadherin gene, which is often downregulated in HCC, leading to increased invasiveness and metastasis [163]. Research also investigated the role of CEBP/α, a tumor suppressor transcription factor, in the inhibition of HCC metastasis [164]. The study utilizes saRNAs to enhance the expression of CEBP/α in vitro and in vivo. The research demonstrates that CEBP/α-saRNA transfection inhibits the migration and invasion of hepatoma cells by suppressing the EMT process [165]. The study highlights the significant downregulation of key EMT markers, such as N-Cadherin, Slug, and Vimentin, alongside the upregulation of E-Cadherin, indicating a reversion to a less invasive epithelial phenotype. Another important target is the p21 gene, a cyclin-dependent kinase inhibitor that plays a crucial role in cell cycle regulation and apoptosis [166]. The expression of p21 is often suppressed in HCC, leading to uncontrolled cell proliferation. Preclinical studies have demonstrated that saRNA targeting the p21 promoter can enhance its expression, leading to cell cycle arrest and increased sensitivity of HCC cells to chemotherapy [167]. LHPP, a recently identified tumor suppressor, has shown promise as a target for therapeutic intervention in HCC. As shown in Figure 8, researchers utilized a systematic screening process to identify effective saRNAs that can upregulate the tumor suppressor gene LHPP in HCC cells [168]. The screening involved designing and synthesizing a library of 290 saRNA candidates, each specifically targeting different regions of the LHPP promoter. One lead saRNA, RAG7-133, demonstrated significant inhibition of tumor growth and enhanced therapeutic efficacy in combination with regorafenib in vitro and in vivo, suggesting that saRNA-mediated LHPP activation could be a novel approach for HCC treatment.
Particularly, saRNA nanotherapeutics are valuable in restoring the function of tumor suppressors and other regulatory genes critical for controlling cell proliferation, apoptosis, and metastasis. Additionally, saRNA therapy can be designed to target multiple genes simultaneously, providing a broader impact on disease. The use of NP delivery systems further enhances the effectiveness of saRNA by protecting the RNA from degradation and ensuring its efficient delivery to target cells. This targeted delivery minimizes off-target effects and reduces the likelihood of systemic side effects, making saRNA nanotherapy a safer alternative to traditional treatments. Moreover, the transient nature of saRNA expression reduces the risk of long-term adverse effects, offering a balance between efficacy and safety.
RNA nanotherapeutics in combination therapy for HCC
When RNA nanotherapeutics is combined with other treatment modalities, it offers a powerful approach to combination therapy for HCC. This strategy leverages the unique capabilities of RNA molecules such as siRNA, miRNA, and mRNA to target specific oncogenes and regulatory pathways, while concurrently employing traditional or novel cancer treatments such as chemotherapy, targeted therapy, immunotherapy, or radiation therapy [169-171]. By combining these approaches, overall therapeutic efficacy is enhanced, and the limitations of individual treatments, such as resistance or toxicity, can be mitigated.
The mechanism of action of RNA nanotherapeutics in combination therapy often involves silencing or modulating genes that promote cancer progression, drug resistance, or immune evasion. For example, siRNA can be used to silence genes responsible for chemotherapy resistance, making cancer cells more susceptible to chemotherapeutic agents [172]. Meanwhile, mRNA can be used to restore the expression of tumor suppressor genes or enhance immune responses against cancer cells [173]. The use of NP delivery ensures that RNA molecules are effectively transported to the tumor site, protected from degradation, and released in a controlled manner, maximizing therapeutic benefit.
The therapeutic potential of LHPP-saRNA in suppressing HCC treatment. (A) Schematic illustration of RNA activation mechanism to upregulate the tumor suppressor LHPP using saRNA in HCC cells. The saRNA forms a complex with Ago2, facilitating targeted LHPP expression and potentially reducing HCC progression. (B) Screening results of saRNA candidates in Huh7 cells, showing relative LHPP mRNA expression for each saRNA tested. (C) Western blot analysis of LHPP, p-AKT, and Akt levels in HCC cells treated with lead saRNAs, demonstrating successful LHPP upregulation and AKT pathway inhibition. (D) Representative images of tumor growth in mouse xenograft models treated with vehicle, RAG7-133, regorafenib, and the combination, showing enhanced anti-tumor effects with RAG7-133 and regorafenib co-treatment. Adapted from [168]. Copyright 2024, Public Library of Science.
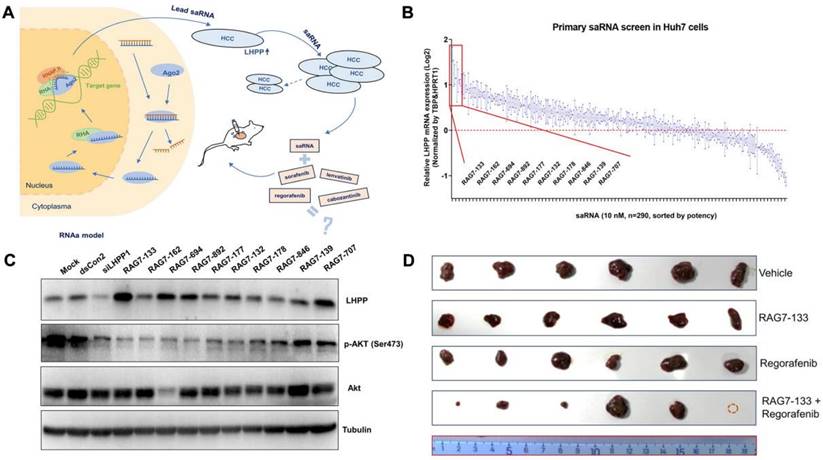
Research on RNA nanotherapeutics in combination with other therapies is an active field, with many promising advances in both preclinical and clinical settings. A notable example is the use of siRNA targeting BCL-2, an anti-apoptotic gene often overexpressed in HCC that contributes to chemotherapy resistance [174]. In preclinical studies, siRNA targeting BCL-2 combined with Sorafenib has shown enhanced cancer cell death and tumor regression, outperforming either treatment alone. This combination approach is being explored in early clinical trials to assess its safety and efficacy in HCC patients.
Another focus of research is the combination of RNA nanotherapeutics with immune checkpoint inhibitors such as anti-PD-1/PD-L1 antibodies. In this approach, a study utilizes a CXCR4 targeted p53 mRNA-loaded nanoparticle, named CTCE-p53 NPs, to restore the function of the tumor suppressor p53 in HCC cells (Figure 9) [27]. These NPs are engineered with PLGA polymer, ionizable lipids, and CTCE-PEG, which specifically targets the TME. The CTCE-p53 NPs not only induce the re-expression of p53, leading to apoptosis in p53-null cancer cells, but also reprogram the immune microenvironment. This reprogramming increases the infiltration of CD8+ T cells and natural killer (NK) cells while reducing the population of immunosuppressive M2-like macrophages, thus enhancing the overall anti-tumor immune response. When combined with anti-PD-1 therapy, the CTCE-p53 NPs significantly amplify the therapeutic effects by overcoming the immune evasion mechanisms typically employed by tumors. This dual strategy effectively suppresses tumor growth more than either treatment alone, highlighting the innovative synergy between RNA nanotherapeutics based nanotherapy and immune checkpoint blockade. The results from this study suggest that combining p53 mRNA nanotherapy with PD-1 inhibition could offer a powerful, complementary approach to treating HCC and potentially other cancers characterized by p53 dysfunction. This combination approach has shown promise in preclinical models, leading to improved tumor control and extended survival in HCC mouse models.
Beyond chemotherapy and immunotherapy, RNA nanotherapeutics is also being combined with targeted therapies such as tyrosine kinase inhibitors (TKIs). For example, siRNA targeting MYC or β-catenin, combined with sorafenib (a commonly used TKI in HCC), has demonstrated synergistic effects in reducing tumor growth and overcoming resistance to Sorafenib [175]. These findings highlight the potential of RNA nanotherapeutics to enhance the effectiveness of existing targeted therapies and provide new treatment options for HCC patients who do not respond to standard treatments.
Combining RNA nanotherapeutics with other treatment modalities offers several advantages [176]. First, it allows for a multifaceted attack on tumors, targeting different aspects of cancer biology simultaneously. This approach helps overcome the limitations of single therapies, such as drug resistance or incomplete tumor eradication. Second, the use of NPs for RNA delivery enhances the stability and bioavailability of RNA molecules, ensuring that they reach the tumor site in sufficient quantities to exert therapeutic effects.
CTCE-p53 NPs for enhancing anti-tumor immune response in HCC. (A) Schematic illustration showing the composition and mechanism of CTCE-p53 NPs in reprogramming the immune microenvironment and enhancing anti-tumor immunity when combined with anti-PD-1 therapy. These NPs upregulate CD4+ and CD8+ T cells, M1 TAMs, and NK cells while downregulating M2 TAMs. (B) TEM image showing the morphology of the CTCE-p53 NPs (scale bar: 200 nm). (C) Western blot analysis confirms the expression of p53 protein in treated HCC cells. (D) Immunofluorescence image of p53 protein expression in p53-knockout RIL-175 cells treated with CTCE-p53 NPs (scale bar: 50 μm). (E) Tumor growth curves in p53-null RIL-175 tumor-bearing mice treated with different formulations. (F) Quantification of CD3+CD8+ T cells infiltrating tumors, and (G) CD206+ M2-like TAMs in tumors, demonstrating enhanced immune response and reduced immunosuppressive TAMs in mice treated with CTCE-p53 NPs combined with anti-PD-1 therapy. Adapted from [27]. Copyright 2022, Springer Nature.
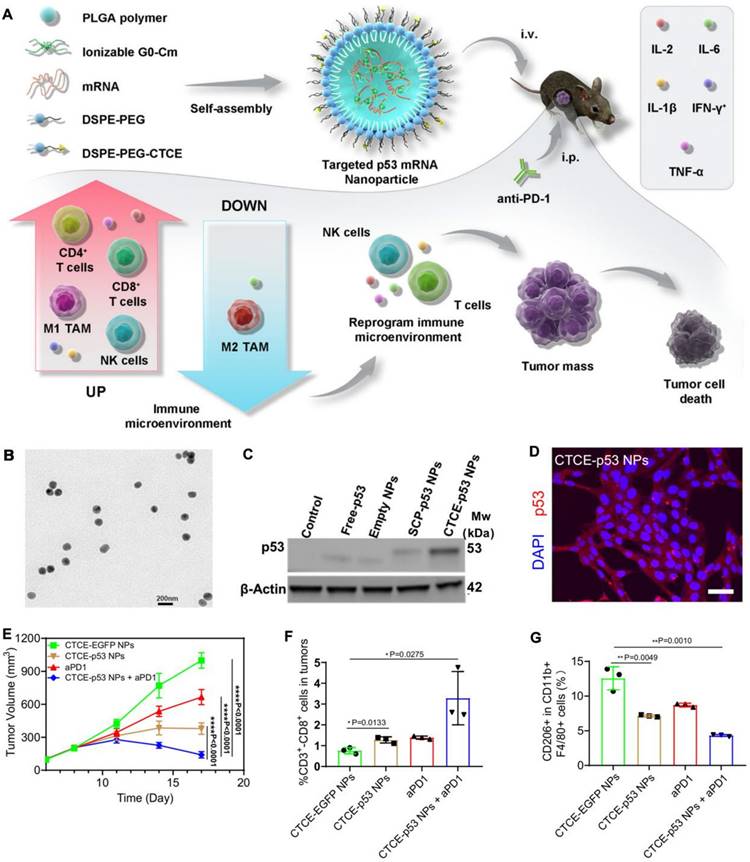
Additionally, combining RNA therapy with other treatments can reduce the required dose of chemotherapy or other drugs, minimizing toxicity and improving the overall safety of the treatment regimen.
RNA nanotherapeutics in combination with other treatments represents a promising strategy for HCC combination therapy. Preclinical and early clinical research has demonstrated the potential of these combination approaches to improve tumor control, overcome resistance, and reduce treatment-related toxicity [177]. As research continues, RNA-based combination therapies are likely to play an increasingly important role in HCC management, offering new hope for more effective and personalized treatment options.
In summary, RNA nanotherapeutics represent a cutting-edge approach for HCC treatment, utilizing nanocarriers to deliver various RNA molecules, such as siRNA, miRNA, mRNA, and saRNA, directly to tumor cells. These therapies are designed to precisely target genetic pathways involved in cancer progression, offering enhanced stability, cellular uptake, and specificity compared to traditional methods. The following Table 2 provides an overview of key examples of RNA nanotherapeutics in HCC treatment, highlighting their mechanisms of action, delivery systems, and therapeutic outcomes.
Outlook
Opportunities and challenges of RNA nanotherapeutics for HCC
While still in various stages of research and clinical development, RNA nanotherapies hold immense potential to provide more effective, personalized, and less toxic treatment options for HCC [179]. However, to fully realize the potential of RNA nanotherapeutics for HCC, several critical challenges in clinical translation must be addressed.
How to achieve efficient and specific delivery of RNA nanotherapeutics
A primary challenge is the efficient and specific delivery of RNA therapies to tumor sites, which requires navigation through a complex TME characterized by a dense extracellular matrix, abnormal vasculature, and immune barriers [180]. Precise targeting of HCC cells is crucial to maximizing therapeutic efficacy while minimizing off-target effects on healthy tissues. RNA molecules are inherently unstable and prone to degradation by nucleases in the bloodstream, and even when encapsulated in NPs, maintaining their stability until they reach target cells remains a significant challenge [181]. Strategies to enhance stability include chemical modifications of RNA or the development of more robust NP formulations, areas that are under active investigation.
Developing targeted delivery systems that utilize ligands or antibodies on NP surfaces to specifically bind to receptors overexpressed on HCC cells, such as ASGPR, GPC3, or EGFR, is essential. Additionally, leveraging the enhanced permeability and retention effect in tumors can improve NP accumulation at the tumor site. Advances in biomimetic delivery systems, such as exosomes that naturally target specific tissues, may also enhance targeting specificity [182]. Enhancing the chemical stability of RNA molecules through modifications such as 2'-O-methyl or 2'-fluoro substitutions can make them more resistant to nuclease degradation [183]. Optimizing NP formulations, including protective polymers or the use of nanocages, can further protect RNA from degradation. Encapsulating RNA in NPs with pH-sensitive or enzyme-responsive release mechanisms ensures that RNA remains stable until it reaches the TME.
Biosafety concerns of the nanocarriers
While NPs offer protection against RNA degradation, they can also provoke immune responses [184], particularly with synthetic delivery systems like LNPs. These immune reactions may activate the innate immune system, resulting in the rapid clearance of the nanoparticles, which compromises therapeutic effectiveness and can lead to adverse effects such as inflammation or allergic reactions. The risk of immune activation is especially pronounced with repeated dosing, which can further amplify immune recognition and result in diminished therapeutic efficacy over time.
To address these challenges, balancing the immunogenicity of delivery systems with their efficacy has become a key focus in nanomedicine development. Refining the composition of LNPs to minimize immunogenicity, such as using ionizable lipids less likely to trigger immune responses, is also crucial [69]. Integrating polyethylene glycol (PEG) coating can reduce the risk of immune system recognition, though care must be taken to avoid the “PEGylation syndrome”, where repeated dosing can lead to immune reactions against PEG.
An emerging solution is the use of biomimetic carriers, such as exosomes or cell membrane-coated nanoparticles, which inherently have lower immunogenicity compared to synthetic nanoparticles [185]. These biomimetic vectors can evade immune detection more effectively due to their natural origin, making them well-suited for repeated administration.
List of representative RNA nanotherapeutics applications in HCC treatment
| RNA type | Vector type | Combination Therapy | Target Receptor | Outcomes | Trail Phase | Ref |
|---|---|---|---|---|---|---|
| miR-26a mimics | Exsome | N/A | N/A | Inhibition of cell proliferation, induced cell cycle arrest | Preclinical | [139] |
| miR-34a mimics | LNPs | N/A | N/A | Targeting MYC and BCL-2, reduced tumor growth, increased apoptosis | Early Clinical Trials | [137] |
| miR-122 mimics | LNPs | N/A | N/A | Restoration of miR-122 levels, tumor growth inhibition | Preclinical | [135] |
| VEGF siRNA | PNPs | 5-FU | VEGFR | Inhibition of angiogenesis, reduced tumor blood supply | Preclinical | [144] |
| MYC siRNA | PNPs | Sorafenib | asialoglycoprotein receptor | Reduced tumor cell proliferation, induced apoptosis | Preclinical | [145] |
| BCL-2 siRNA | PNPs | N/A | N/A | Enhanced cancer cell death, tumor regression | Preclinical | [147] |
| β-catenin siRNA | LNPs | Sorafenib | β-catenin receptor | Reduced tumor growth, overcoming Sorafenib resistance | Preclinical | [148] |
| ALN-VSP | LNPs | N/A | N/A | Well-tolerated and prolonged disease stabilization in participants | Phase 1 | [146] |
| MFAP-5 siRNA | PNPs | Desloratadine | N/A | Significant tumor burden reduction, inhibited angiogenesis | Preclinical | [149] |
| IL-12 mRNA | LNPs | N/A | Not specified | Immune modulation, suppression of tumorigenesis | Preclinical | [153] |
| p53 mRNA | PNPs | Anti-PD-1 | CXCR4 receptor | Restoration of p53 expression, enhanced immune response | Preclinical | [27] |
| OX40L mRNA | LNPs | N/A | N/A | Inhibits tumor growth, increases CD4+ and CD8+ T cell populations, promotes immune infiltration | Preclinical | [178] |
| Bims mRNA | ALPPL2-Binding Peptide | N/A | ALPPL2 | Enhanced targeted delivery, significant tumor growth inhibition | Preclinical | [156] |
| CEBPA saRNA | SMARTICLES | TKIs | N/A | Upregulation of CEBPA, tumor shrinkage, improved liver function | Phase I | [63] |
| CEBPA saRNA | Lipopolyplex | N/A | N/A | Gene activation, tumor growth inhibition in colorectal cancer model | Preclinical | [165] |
| p21 saRNA | Lipopolyplex | N/A | N/A | Cell cycle arrest and inhibition of invasion and migration | Preclinical | [167] |
Additionally, surface modifications such as incorporating self-peptides or anti-inflammatory molecules can further reduce immune recognition.
Moreover, the integration of machine learning into the discovery and development of LNPs significantly enhances the precision and efficiency of mRNA delivery systems [186, 187]. Machine learning offers several advantages, such as the ability to process vast datasets and identify optimal ionizable lipids, which are critical for mRNA delivery. By combining machine learning with advanced combinatorial chemistry, researchers can rapidly explore extensive libraries of potential lipid candidates, accelerating the identification of lipids that enhance transfection efficacy and stability. This approach not only expedites the development of effective LNPs but also allows for the fine-tuning of LNP formulations to address specific therapeutic needs.
How to design personalized and adaptive approaches for overcoming HCC heterogeneity
HCC is a highly heterogeneous disease, with significant genetic and epigenetic variations between tumors and even within different regions of the same tumor [188]. This intratumoral and intertumoral heterogeneity significantly complicates treatment efforts, as these variations can influence the tumor's response to therapies and promote resistance. The inherent diversity of HCC results in the emergence of resistant cancer cell subpopulations, even in the presence of otherwise effective treatment. Consequently, overcoming this heterogeneity is one of the most pressing challenges in advancing effective HCC therapies. To meet this challenge, personalized and adaptive treatment approaches are essential.
One promising approach is the discovery of new HCC-related genes through clinical analysis, which can provide a basis for developing personalized RNA-based therapeutics. Techniques such as next-generation sequencing (NGS), single-cell RNA sequencing (scRNA-seq), and whole-genome methylation analysis can be employed to identify critical genetic and epigenetic alterations in individual HCC patients [189]. By examining patient-derived tumor samples, novel oncogenes and tumor suppressor genes that contribute to disease progression can be identified. This knowledge allows for the precise design of RNA therapeutics tailored to modulate specific gene expression patterns. The use of bioinformatics tools, such as machine learning algorithms, can further aid in the discovery and validation of these gene targets [190]. Machine learning approaches can identify gene expression patterns that correlate with poor prognosis or treatment resistance, thus helping to prioritize targets for RNA-based intervention. This process of correlating clinical data with specific genetic mutations or expression levels can guide the design of co-related RNA therapeutics, maximizing therapeutic efficacy while minimizing off-target effects.
Therefore, by analyzing the genetic and molecular characteristics of each patient's tumor, personalized medicine approaches can tailor RNA-based therapies to individual needs [191]. This can include using siRNA or miRNA to target specific oncogenic pathways, or mRNA or saRNA to enhance tumor suppressor activity, thereby providing more precise and effective treatment while reducing off-target effects. Combination therapies targeting multiple pathways simultaneously, such as using siRNA in combination with chemotherapy or immune checkpoint inhibitors, can help overcome resistance and address tumor heterogeneity. The development of adaptive treatment regimens that evolve with changes in tumor biology can further improve long-term efficacy [192], ensuring that therapies remain effective even as the disease progresses. Integrating these innovations with machine learning-enhanced LNP discovery can lead to more effective and personalized RNA-based nanotherapies, optimizing therapeutic outcomes for patients.
Conclusion
RNA nanotherapeutics represent an innovative approach in HCC treatment, harnessing the precision of RNA molecules such as siRNA, miRNA, mRNA, and saRNA, in combination with advanced NP delivery systems to specifically target cancer cells. These therapies offer the potential to silence oncogenes, restore tumor suppressor functions, and modulate immune responses, providing a highly targeted approach that may overcome the high toxicity, limited specificity, and drug resistance associated with conventional treatments. By personalizing therapy to address specific genetic and molecular alterations in individual tumors, RNA nanotherapeutics can effectively tackle the heterogeneity inherent in HCC, enhancing treatment efficacy while minimizing off-target effects.
To achieve successful clinical translation of RNA nanotherapeutics, a multifaceted strategy is required. This includes conducting thorough scientific research to optimize delivery systems and ensure safety, collaborating with regulatory agencies to establish clear approval pathways, developing scalable manufacturing processes for widespread accessibility, strategically integrating these therapies into clinical practice, potentially in combination with existing treatments. By focusing on these critical areas, the medical community can advance RNA nanotherapeutics toward becoming a viable and impactful option for patients battling HCC, ultimately improving outcomes and offering new hope in the management of this challenging disease.
In summary, recognizing the burgeoning trend towards developing more precise and functional nanocarriers, we explore how these cutting-edge strategies can enhance tumor specificity and RNA accumulation, thereby facilitating further clinical translation and advancing cancer therapy. As strides are made in nanotechnology and our understanding of cancer deepens, we believe that these RNA nanotherapeutics will not only overcome the limitations of conventional treatments but also set a new benchmark in the next generation of nano-anticancer agents. Ultimately, this review aims to highlight the potential of RNA nanotherapeutics to become a paragon in personalized medicine for HCC, offering hope for more effective and less toxic treatment options.
Abbreviations
HCC: Hepatocellular carcinoma; LNP: lipid nanoparticle; PNP: polymer nanoparticle; miRNA: micro RNA; siRNA: small interfering RNA; mRNA: message RNA; saRNA: small activating RNA; RNA interference: RNAi; TME: tumor microenvironment; EV: Extracellular vesicle; Virus-like particle: VLP; adeno-associated viruses: AAV; LSEC: liver sinusoidal endothelial cells; extracellular matrix: ECM; Myeloid-derived suppressor cells: MDSCs; Cancer-associated fibroblasts: CAFs; Epithelial-mesenchymal transition: EMT; asialoglycoprotein receptor: ASGPR; N-acetylgalactosamine: GalNAc; Glypican-3: GPC3; RNA-induced silencing complex: RISC; Vascular endothelial growth factor: VEGF; Polyion complex micelles: PICMs; Microfibrillar-associated protein 5: MFAP-5; Tumor-associated antigens: TAAs; Major histocompatibility complex: MHC; Tekmira-Pololike Kinase 1: TKM-PLK; epidermal growth factor receptor: EGFR; poly(lactic-co-glycolic acid): PLGA; polyethylenimine: PEI; matrix metalloproteinase: MMP; glucose-6-phosphatase-α: G6Pase-α.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (NSFC) (82272852 and 82202330), Nanchong Science and Technology Plan Project (23JCYJPT0043), and China Postdoctoral Science Foundation (2023T160383 and 2023MD734153).
Competing Interests
The authors have declared that no competing interest exists.
References
1. Yang JD, Heimbach J. New advances in the diagnosis and management of hepatocellular carcinoma. BMJ. 2020;371:m3544
2. Cassinotto C, Nogue E, Durand Q, Panaro F, Assenat E, Dohan A. et al. Life expectancy of patients with hepatocellular carcinoma according to the upfront treatment: A nationwide analysis. Diagn Interv Imag. 2023;104:192-9
3. Singal AG, Kanwal F, Llovet JM. Global trends in hepatocellular carcinoma epidemiology: implications for screening, prevention and therapy. Nat Rev Clin Oncol. 2023;20:864-84
4. Yang C, Zhang H, Zhang L, Zhu AX, Bernards R, Qin W. et al. Evolving therapeutic landscape of advanced hepatocellular carcinoma. Nat Rev Gastro Hepat. 2023;20:203-22
5. Singal AG, Llovet JM, Yarchoan M, Mehta N, Heimbach JK, Dawson LA. et al. AASLD practice guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023;78:1922-65
6. Ladd AD, Duarte S, Sahin I, Zarrinpar A. Mechanisms of drug resistance in HCC. Hepatology. 2024;79:926-40
7. Tan DJH, Tang ASP, Lim WH, Ng CH, Nah B, Fu C. et al. Survival Trends in Sorafenib for Advanced Hepatocellular Carcinoma: A Reconstructed Individual Patient Data Meta-Analysis of Randomized Trials. Liver Cancer. 2023;12:445-56
8. Bhat GR, Sethi I, Sadida HQ, Rah B, Mir R, Algehainy N. et al. Cancer cell plasticity: From cellular, molecular, and genetic mechanisms to tumor heterogeneity and drug resistance. Cancer Metast Rev. 2024;43:197-228
9. Maleki EH, Bahrami AR, Matin M. Cancer cell cycle heterogeneity as a critical determinant of therapeutic resistance. Genes Dis. 2024;11:189-204
10. Hernandez-Gea V, Toffanin S, Friedman SL, Llovet J. Role of the microenvironment in the pathogenesis and treatment of hepatocellular carcinoma. Gastroenterology. 2013;144:512-27
11. Mudd TW, Guddati AKJAjocr. Management of hepatotoxicity of chemotherapy and targeted agents. Am J Cancer Res. 2021;11:3461
12. Pandey PR, Young KH, Kumar D, Jain N. RNA-mediated immunotherapy regulating tumor immune microenvironment: next wave of cancer therapeutics. Mol Cancer. 2022;21:58
13. Liu C, Shi Q, Huang X, Koo S, Kong N, Tao W. mRNA-based cancer therapeutics. Nat Rev Cancer. 2023;23:526-43
14. Zhang X, Xie K, Zhou H, Wu Y, Li C, Liu Y. et al. Role of non-coding RNAs and RNA modifiers in cancer therapy resistance. Mol Cancer. 2020;19:1-26
15. Guerrini G, Magrì D, Gioria S, Medaglini D, Calzolai L. Characterization of nanoparticles-based vaccines for COVID-19. Nat Nanotechnol. 2022;17:570-576
16. Yan Y, Liu X-Y, Lu A, Wang X-Y, Jiang L-X, Wang J. Non-viral vectors for RNA delivery. J Control Release. 2022;342:241-79
17. Zhu X, Tao W, Liu D, Wu J, Guo Z, Ji X. et al. Surface De-PEGylation controls nanoparticle-mediated siRNA delivery in vitro and in vivo. Theranostics. 2017;7:1990
18. Zhang Y, Luo J, Gui X, Zheng Y, Schaar E, Liu G. et al. Bioengineered nanotechnology for nucleic acid delivery. J Control Release. 2023;364:124-41
19. Veiga N, Diesendruck Y, Peer D. Targeted lipid nanoparticles for RNA therapeutics and immunomodulation in leukocytes. Adv Drug Deliv Rev. 2020;159:364-76
20. Zhou S, Ma Y, Liu X, Yu P, Huang N, Song L. et al. Targeted Delivery of Glypican 3 (GPC3) Antibody-Modified MicroRNA (miR let-7b-5p) Polymer Nanoparticles to Sorafenib-Resistant Hepatsocellular Carcinoma Cells. J Biomed Nanotechnol. 2021;17:677-90
21. Xiao Y, Xu Z, Cheng Y, Huang R, Xie Y, Tsai HI. et al. Fe(3+)-binding transferrin nanovesicles encapsulating sorafenib induce ferroptosis in hepatocellular carcinoma. Biomater Res. 2023;27:63
22. Zimmermann TS, Karsten V, Chan A, Chiesa J, Boyce M, Bettencourt BR. et al. Clinical proof of concept for a novel hepatocyte-targeting GalNAc-siRNA conjugate. Mol Ther. 2017;25:71-8
23. Hattab D, Gazzali AM, Bakhtiar A. Clinical advances of siRNA-based nanotherapeutics for cancer treatment. Pharmaceutics. 2021;13:1009
24. Daige CL, Wiggins JF, Priddy L, Nelligan-Davis T, Zhao J, Brown D. Systemic delivery of a miR34a mimic as a potential therapeutic for liver cancer. Mol Cancer Ther. 2014;13:2352-60
25. Sarker D, Plummer R, Meyer T, Sodergren MH, Basu B, Chee CE. et al. MTL-CEBPA, a small activating RNA therapeutic upregulating C/EBP-α, in patients with advanced liver cancer: a first-in-human, multicenter, open-label, phase I trial. Clin Cancer Res. 2020;26:3936-46
26. Kong N, Tao W, Ling X, Wang J, Xiao Y, Shi S. et al. Synthetic mRNA nanoparticle-mediated restoration of p53 tumor suppressor sensitizes p53-deficient cancers to mTOR inhibition. Sci Transl Med. 2019;11:eaaw1565
27. Xiao Y, Chen J, Zhou H, Zeng X, Ruan Z, Pu Z. et al. Combining p53 mRNA nanotherapy with immune checkpoint blockade reprograms the immune microenvironment for effective cancer therapy. Nat Commun. 2022;13:758
28. Chen Z, Xie H, Hu M, Huang T, Hu Y, Sang N. et al. Recent progress in treatment of hepatocellular carcinoma. Am J Cancer Res. 2020;10:2993
29. Giannelli G, Rani B, Dituri F, Cao Y, Palasciano G. Moving towards personalised therapy in patients with hepatocellular carcinoma: the role of the microenvironment. Gut. 2014;63:1668-76
30. Wei L, Wang X, Lv L, Liu J, Xing H, Song Y. et al. The emerging role of microRNAs and long noncoding RNAs in drug resistance of hepatocellular carcinoma. Mol Cancer. 2019;18:1-11
31. Cring MR, Sheffield VC. Gene therapy and gene correction: targets, progress, and challenges for treating human diseases. Gene Ther. 2022;29:3-12
32. Khorkova O, Stahl J, Joji A, Volmar C-H, Wahlestedt C. Amplifying gene expression with RNA-targeted therapeutics. Nat Rev Drug Discov. 2023;22:539-61
33. Saliminejad K, Khorram Khorshid HR, Soleymani Fard S, Ghaffari SH. An overview of microRNAs: Biology, functions, therapeutics, and analysis methods. J Cell Physiol. 2019;234:5451-65
34. Soifer HS, Rossi JJ, Sætrom P. MicroRNAs in disease and potential therapeutic applications. Mol Ther. 2007;15:2070-79
35. Babashah S, Soleimani M. The oncogenic and tumour suppressive roles of microRNAs in cancer and apoptosis. Eur J Cancer. 2011;47:1127-37
36. Boca S, Gulei D, Zimta A-A, Onaciu A, Magdo L, Tigu AB. et al. Nanoscale delivery systems for microRNAs in cancer therapy. Cell Mol Life Sci. 2020;77:1059-86
37. To KK, Fong W, Tong CW, Wu M, Yan W, Cho WC. Advances in the discovery of microRNA-based anticancer therapeutics: latest tools and developments. Expert Opin Drug Discov. 2020;15:63-83
38. Zapletal D, Kubicek K, Svoboda P, Stefl R. Dicer structure and function: conserved and evolving features. EMBO Rep. 2023;24:e57215
39. Wang P, Zhou Y, Richards AM. Effective tools for RNA-derived therapeutics: siRNA interference or miRNA mimicry. Theranostics. 2021;11:8771
40. Qiao M, Zeng C, Liu C, Lei Z, Liu B, Xie H. The advancement of siRNA-based nanomedicine for tumor therapy. Nanomedicine. 2024:1-22
41. Ali Zaidi SS, Fatima F, Ali Zaidi SA, Zhou D, Deng W, Liu SJ. Engineering siRNA therapeutics: challenges and strategies. J Nanobiotechnol. 2023;21:381
42. Jadhav V, Vaishnaw A, Fitzgerald K, Maier MAJNB. RNA interference in the era of nucleic acid therapeutics. Nat Biotechnol. 2024;42:394-405
43. Shen G, Liu J, Yang H, Xie N, Yang Y. mRNA therapies: Pioneering a new era in rare genetic disease treatment. J Control Release. 2024;369:696-721
44. Witzigmann D, Kulkarni JA, Leung J, Chen S, Cullis PR, van der Meel R. Lipid nanoparticle technology for therapeutic gene regulation in the liver. Adv Drug Deliv Rev. 2020;159:344-63
45. Han G, Noh D, Lee H, Lee S, Kim S, Yoon HY. et al. Advances in mRNA therapeutics for cancer immunotherapy: From modification to delivery. Adv Drug Deliv Rev. 2023;199:114973
46. Meganck RM, Baric RS. Developing therapeutic approaches for twenty-first-century emerging infectious viral diseases. Nat Med. 2021;27:401-10
47. Rohner E, Yang R, Foo KS, Goedel A, Chien KR. Unlocking the promise of mRNA therapeutics. Nat Biotechnol. 2022;40:1586-600
48. Khurana A, Allawadhi P, Khurana I, Allwadhi S, Weiskirchen R, Banothu AK. et al. Role of nanotechnology behind the success of mRNA vaccines for COVID-19. Nano Today. 2021;38:101142
49. Chaudhary N, Weissman D, Whitehead KA. mRNA vaccines for infectious diseases: principles, delivery and clinical translation. Nat Rev Drug Discov. 2021;20:817-38
50. Beck JD, Reidenbach D, Salomon N, Sahin U, Türeci Ö, Vormehr M. et al. mRNA therapeutics in cancer immunotherapy. Mol Cancer. 2021;20:69
51. Heine A, Juranek S, Brossart P. Clinical and immunological effects of mRNA vaccines in malignant diseases. Mol Cancer. 2021;20:1-20
52. Huang X, Kong N, Zhang X, Cao Y, Langer R, Tao W. The landscape of mRNA nanomedicine. Nat Med. 2022;28:2273-87
53. Wang Y-S, Kumari M, Chen G-H, Hong M-H, Yuan JP-Y, Tsai J-L. et al. mRNA-based vaccines and therapeutics: An in-depth survey of current and upcoming clinical applications. J Biomed Sci. 2023;30:84
54. Eftekhari Z, Zohrabi H, Oghalaie A, Ebrahimi T, Shariati FS, Behdani M. et al. Advancements and Challenges in mRNA and Ribonucleoprotein-Based Therapies: From Delivery Systems to Clinical Applications. Mol Ther-Nucl Acids. 2024;3:102313
55. Kwok A, Raulf N, Habib N. Developing small activating RNA as a therapeutic: current challenges and promises. Ther Deliv. 2019;10:151-64
56. Kingwell K. Small activating RNAs lead the charge to turn up gene expression. Nat Rev Drug Discov. 2021;20:573-74
57. Ghanbarian H, Aghamiri S, Eftekhary M, Wagner N, Wagner KD. Small Activating RNAs: Towards the Development of New Therapeutic Agents and Clinical Treatments. Cells. 2021;10:591
58. Zheng L, Wang L, Gan J, Zhang H. RNA activation: promise as a new weapon against cancer. Cancer Lett. 2014;355:18-24
59. Bakrania A, Mo Y, Zheng G, Bhat M. RNA nanomedicine in liver diseases. Hepatology. 2024;10:1097
60. Tan CP, Sinigaglia L, Gomez V, Nicholls J, Habib NA. RNA Activation-A Novel Approach to Therapeutically Upregulate Gene Transcription. Molecules. 2021;26:6530
61. Zhao Y, Shu R, Liu J. The development and improvement of ribonucleic acid therapy strategies. Mol Ther Nucleic Acids. 2021;26:997-1013
62. Reebye V, Huang KW, Lin V, Jarvis S, Cutilas P, Dorman S. et al. Gene activation of CEBPA using saRNA: preclinical studies of the first in human saRNA drug candidate for liver cancer. Oncogene. 2018;37:3216-28
63. Sadagopan N, He AR. Recent Progress in Systemic Therapy for Advanced Hepatocellular Carcinoma. Int J Mol Sci. 2024;25:1259
64. Halloy F, Biscans A, Bujold KE, Debacker A, Hill AC, Lacroix A. et al. Innovative developments and emerging technologies in RNA therapeutics. RNA Biol. 2022;19:313-32
65. Dammes N, Peer D. Paving the Road for RNA Therapeutics. Trends Pharm Sci. 2020;41:755-75
66. Ryu JH, Koo H, Sun IC, Yuk SH, Choi K, Kim K. et al. Tumor-targeting multi-functional nanoparticles for theragnosis: new paradigm for cancer therapy. Adv Drug Deliv Rev. 2012;64:1447-58
67. Li C, Samulski RJ. Engineering adeno-associated virus vectors for gene therapy. Nat Rev Genet. 2020;21:255-72
68. Wang C, Pan C, Yong H, Wang F, Bo T, Zhao Y. et al. Emerging non-viral vectors for gene delivery. J Nanobiotechnol. 2023;21:272
69. Eygeris Y, Gupta M, Kim J, Sahay G. Chemistry of Lipid Nanoparticles for RNA Delivery. Acc Chem Res. 2022;55:2-12
70. El-Kharrag R, Berckmueller KE, Madhu R, Cui M, Campoy G, Mack HM. et al. Efficient polymer nanoparticle-mediated delivery of gene editing reagents into human hematopoietic stem and progenitor cells. Mol Ther. 2022;30:2186-98
71. Al Sharabati M, Sabouni R, Husseini GA. Biomedical Applications of Metal-Organic Frameworks for Disease Diagnosis and Drug Delivery: A Review. Nanomaterials. 2022;12:277
72. Bulcha JT, Wang Y, Ma H, Tai PWL, Gao G. Viral vector platforms within the gene therapy landscape. Signal Transduct Target Ther. 2021;6:53
73. Wang S, Liang B, Wang W, Li L, Feng N, Zhao Y. et al. Viral vectored vaccines: design, development, preventive and therapeutic applications in human diseases. Signal Transduct Target Ther. 2023;8:149
74. Li X, Le Y, Zhang Z, Nian X, Liu B, Yang X. Viral Vector-Based Gene Therapy. Int J Mol Sci. 2023;24:7736
75. Kang L, Jin S, Wang J, Lv Z, Xin C, Tan C. et al. AAV vectors applied to the treatment of CNS disorders: Clinical status and challenges. J Control Release. 2023;355:458-73
76. Croze RH, Kotterman M, Burns CH, Schmitt CE, Quezada M, Schaffer D. et al. Viral Vector Technologies and Strategies: Improving on Nature. Int Ophthalmol Clin. 2021;61:59-89
77. Mohanty R, Chowdhury CR, Arega S, Sen P, Ganguly P, Ganguly N. CAR T cell therapy: A new era for cancer treatment. Oncol Rep. 2019;42:2183-95
78. Ghosh S, Brown AM, Jenkins C, Campbell K. Viral Vector Systems for Gene Therapy: A Comprehensive Literature Review of Progress and Biosafety Challenges. Appl Biosaf. 2020;25:7-18
79. Loo YS, Bose RJ, McCarthy JR, Mat Azmi ID, Madheswaran T. Biomimetic bacterial and viral-based nanovesicles for drug delivery, theranostics, and vaccine applications. Drug Discov Today. 2021;26:902-15
80. Segel M, Lash B, Song J, Ladha A, Liu CC, Jin X. et al. Mammalian retrovirus-like protein PEG10 packages its own mRNA and can be pseudotyped for mRNA delivery. Science. 2021;373:882-89
81. Fuenmayor J, Gòdia F, Cervera L. Production of virus-like particles for vaccines. N Biotechnol. 2017;39:174-80
82. Yang Z, Shi J, Xie J, Wang Y, Sun J, Liu T. et al. Large-scale generation of functional mRNA-encapsulating exosomes via cellular nanoporation. Nat Biomed Eng. 2020;4:69-83
83. Elewaily MI, Elsergany AR. Emerging role of exosomes and exosomal microRNA in cancer: pathophysiology and clinical potential. J Cancer Res Clin Oncol. 2021;147:637-48
84. Yoo JW, Irvine DJ, Discher DE, Mitragotri S. Bio-inspired, bioengineered and biomimetic drug delivery carriers. Nat Rev Drug Discov. 2011;10:521-35
85. Kurakula H, Vaishnavi S, Sharif MY, Ellipilli S. Emergence of Small Interfering RNA-Based Gene Drugs for Various Diseases. ACS omega. 2023;8:20234-50
86. Mokhtarzadeh A, Alibakhshi A, Hashemi M, Hejazi M, Hosseini V, de la Guardia M. et al. Biodegradable nano-polymers as delivery vehicles for therapeutic small non-coding ribonucleic acids. J Control Release. 2017;245:116-26
87. Thomas TJ, Tajmir-Riahi HA, Pillai CKS. Biodegradable Polymers for Gene Delivery. Molecules. 2019;24:3744
88. Kumar R, Santa Chalarca CF, Bockman MR, Bruggen CV, Grimme CJ, Dalal RJ. et al. Polymeric Delivery of Therapeutic Nucleic Acids. Chem Rev. 2021;121:11527-652
89. Younis MA, Tawfeek HM, Abdellatif AAH, Abdel-Aleem JA, Harashima H. Clinical translation of nanomedicines: Challenges, opportunities, and keys. Adv Drug Deliv Rev. 2022;181:114083
90. Kargaard A, Sluijter JPG, Klumperman B. Polymeric siRNA gene delivery-transfection efficiency versus cytotoxicity. J Control Release. 2019;316:263-91
91. Lin G, Zhou J, Cheng H, Liu G. Smart Nanosystems for Overcoming Multiple Biological Barriers in Cancer Nanomedicines Transport: Design Principles, Progress, and Challenges. Small. 2023;19:e2207973
92. Wegner KD, Hildebrandt N. Quantum dots: bright and versatile in vitro and in vivo fluorescence imaging biosensors. Chem Soc Rev. 2015;44:4792-834
93. Yang Y, Zhang M, Song H, Yu C. Silica-Based Nanoparticles for Biomedical Applications: From Nanocarriers to Biomodulators. Acc Chem Res. 2020;53:1545-56
94. Kubes P, Jenne C. Immune responses in the liver. Annu Rev Immunol. 2018;36:247-77
95. Du K, Li S, Li C, Li P, Miao C, Luo T. et al. Modeling nonalcoholic fatty liver disease on a liver lobule chip with dual blood supply. Acta Biomater. 2021;134:228-39
96. Gracia-Sancho J, Caparrós E, Fernández-Iglesias A, Francés R. Role of liver sinusoidal endothelial cells in liver diseases. Nat Rev Gastro Hepat. 2021;18:411-31
97. Bennett H, Troutman TD, Sakai M, Glass CK. Epigenetic regulation of kupffer cell function in health and disease. Front Immunol. 2021;11:609618
98. Yang F, Li H, Li Y, Hao Y, Wang C, Jia P. et al. Crosstalk between hepatic stellate cells and surrounding cells in hepatic fibrosis. Int Immunopharmacol. 2021;99:108051
99. Satriano L, Lewinska M, Rodrigues PM, Banales JM, Andersen J B. Metabolic rearrangements in primary liver cancers: cause and consequences. Nat Rev Gastro Hepat. 2019;16:748-66
100. Hu M, Huang L. Nanomaterial manipulation of immune microenvironment in the diseased liver. Adv Funct Mater. 2019;29:1805760
101. Jiang K, Tian K, Yu Y, Wu E, Yang M, Pan F. et al. Kupffer cells determine intrahepatic traffic of PEGylated liposomal doxorubicin. Nat Commun. 2024;15:6136
102. Ning B, Yu D, Yu A-M. Advances and challenges in studying noncoding RNA regulation of drug metabolism and development of RNA therapeutics. Biochem Pharmacol. 2019;169:113638
103. Fu L, Zhang Y, Farokhzad RA, Mendes BB, Conde J, Shi J. 'Passive'nanoparticles for organ-selective systemic delivery: design, mechanism and perspective. Chem Soc Rev. 2023;52:7579-601
104. Torbenson MS. Hepatocellular carcinoma: making sense of morphological heterogeneity, growth patterns, and subtypes. Hum Pathol. 2021;112:86-101
105. Frates MC, Benson CB, Doubilet PM, Kunreuther E, Contreras M, Cibas ES. et al. Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocr Metab. 2006;91:3411-7
106. McWilliams A, Tammemagi MC, Mayo JR, Roberts H, Liu G, Soghrati K. et al. Probability of cancer in pulmonary nodules detected on first screening CT. New Engl J Med. 2013;369:910-9
107. Wei X, Chen Y, Jiang X, Peng M, Liu Y, Mo Y. et al. Mechanisms of vasculogenic mimicry in hypoxic tumor microenvironments. Mol Cancer. 2021;20:1-18
108. Muz B, De La Puente P, Azab F, Kareem Azab A. The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia. 2015;3:83-92
109. De Gaetano V, Pallozzi M, Cerrito L, Santopaolo F, Stella L, Gasbarrini A. et al. Management of Portal Hypertension in Patients with Hepatocellular Carcinoma on Systemic Treatment: Current Evidence and Future Perspectives. Cancers. 2024;16:1388
110. Sas Z, Cendrowicz E, Weinhäuser I, Rygiel TP. Tumor microenvironment of hepatocellular carcinoma: challenges and opportunities for new treatment options. Int J Mol Sci. 2022;23:3778
111. Donne R, Lujambio A. The liver cancer immune microenvironment: Therapeutic implications for hepatocellular carcinoma. Hepatology. 2023;77:1773-96
112. Chen C, Wang Z, Ding Y, Qin Y. Tumor microenvironment-mediated immune evasion in hepatocellular carcinoma. Front Immunol. 2023;14:1133308
113. Xu H, Zhao J, Li J, Zhu Z, Cui Z, Liu R. et al. Cancer associated fibroblast-derived CCL5 promotes hepatocellular carcinoma metastasis through activating HIF1α/ZEB1 axis. Cell Death Dis. 2022;13:478
114. Kobayashi H, Enomoto A, Woods SL, Burt AD, Takahashi M, Worthley DL. et al. Cancer-associated fibroblasts in gastrointestinal cancer. Nat Rev Gastro Hepat. 2019;16:282-95
115. Fan D, Cao Y, Cao M, Wang Y, Cao Y, Gong T. et al. Nanomedicine in cancer therapy. Signal Transduct Target Ther. 2023;8:293
116. Lin Y-X, Wang Y, Blake S, Yu M, Mei L, Wang H. et al. RNA nanotechnology-mediated cancer immunotherapy. Theranostics. 2020;10:281
117. Watson ME, Diepeveen LA, Stubbs KA, Yeoh GC. Glycosylation-related diagnostic and therapeutic drug target markers in hepatocellular carcinoma. J Gastrointestin Liver Dis. 2015;24:349-57
118. Kim Y, Hyun JY, Shin I. Multivalent glycans for biological and biomedical applications. Chem Soc Rev. 2021;50:10567-93
119. Shah S, Famta P, Bagasariya D, Charankumar K, Sikder A, Kashikar R. et al. Tuning Mesoporous Silica Nanoparticles in Novel Avenues of Cancer Therapy. Mol Pharm. 2022;19:4428-52
120. Wei Y, Gu X, Cheng L, Meng F, Storm G, Zhong Z. Low-toxicity transferrin-guided polymersomal doxorubicin for potent chemotherapy of orthotopic hepatocellular carcinoma in vivo. Acta Biomater. 2019;92:196-204
121. Kumar A, Das SK, Emdad L, Fisher PB. Applications of tissue-specific and cancer-selective gene promoters for cancer diagnosis and therapy. Adv Cancer Res. 2023;160:253-315
122. Vyas K, Patel MM. Insights on drug and gene delivery systems in liver fibrosis. Asian J Pharm Sci. 2023;18:100779
123. Saiding Q, Zhang Z, Chen S, Xiao F, Chen Y, Li Y. et al. Nano-bio interactions in mRNA nanomedicine: Challenges and opportunities for targeted mRNA delivery. Adv Drug Deliv Rev. 2023;203:115116
124. Negut I, Bita B. Polymeric Micellar Systems-A Special Emphasis on "Smart" Drug Delivery. Pharmaceutics. 2023;15:976
125. Roy AM, Iyer R, Chakraborty S. The extracellular matrix in hepatocellular carcinoma: Mechanisms and therapeutic vulnerability. Cell Rep Med. 2023;4:101170
126. Lu S, Zhang C, Wang J, Zhao L, Li G. Research progress in nano-drug delivery systems based on the characteristics of the liver cancer microenvironment. Biomed Pharm. 2024;170:116059
127. Dilliard SA, Siegwart DJ. Passive, active and endogenous organ-targeted lipid and polymer nanoparticles for delivery of genetic drugs. Nat Rev Mater. 2023;8:282-300
128. Bai S, Lu Z, Jiang Y, Shi X, Xu D, Shi Y. et al. Nanotransferrin-Based Programmable Catalysis Mediates Three-Pronged Induction of Oxidative Stress to Enhance Cancer Immunotherapy. ACS Nano. 2022;16:997-1012
129. Shi X, Zhang Y, Tian Y, Xu S, Ren E, Bai S. et al. Multi-Responsive Bottlebrush-Like Unimolecules Self-Assembled Nano-Riceball for Synergistic Sono-Chemotherapy. Small Methods. 2021;5:e2000416
130. Wang G, Zhang M, Lai W, Gao Y, Liao S, Ning Q. et al. Tumor Microenvironment Responsive RNA Drug Delivery Systems: Intelligent Platforms for Sophisticated Release. Mol Pharm. 2024;21:4217-37
131. Luo QQ, Tian Y, Qu GJ, Kun H, Luo SS. Functional mechanism and clinical implications of miR-141 in human cancers. Cell Signal. 2022;95:110354
132. Xue J, Niu YF, Huang J, Peng G, Wang LX, Yang YH. et al. miR-141 suppresses the growth and metastasis of HCC cells by targeting E2F3. Tumour Biol. 2014;35:12103-7
133. Kim MK, Moon YA, Song CK, Baskaran R, Bae S, Yang SG. Tumor-suppressing miR-141 gene complex-loaded tissue-adhesive glue for the locoregional treatment of hepatocellular carcinoma. Theranostics. 2018;8:3891-901
134. Sendi H, Yazdimamaghani M, Hu M, Sultanpuram N, Wang J, Moody AS. et al. Nanoparticle Delivery of miR-122 Inhibits Colorectal Cancer Liver Metastasis. Cancer Res. 2022;82:105-13
135. Hsu SH, Yu B, Wang X, Lu Y, Schmidt CR, Lee RJ. et al. Cationic lipid nanoparticles for therapeutic delivery of siRNA and miRNA to murine liver tumor. Nanomedicine. 2013;9:1169-80
136. Rong J, Liu T, Yin X, Shao M, Zhu K, Li B. et al. Co-delivery of camptothecin and MiR-145 by lipid nanoparticles for MRI-visible targeted therapy of hepatocellular carcinoma. J Exper Clin Cancer Res. 2024;43:247
137. Hong DS, Kang YK, Borad M, Sachdev J, Ejadi S, Lim HY. et al. Phase 1 study of MRX34, a liposomal miR-34a mimic, in patients with advanced solid tumours. Brit J Cancer. 2020;122:1630-7
138. Hu J, Liu WF, Zhang XY, Shi GM, Yang XR, Zhou KQ. et al. Synthetic miR-26a mimics delivered by tumor exosomes repress hepatocellular carcinoma through downregulating lymphoid enhancer factor 1. Hepatol Int. 2023;17:1265-78
139. Parvin R, Zhang L, Zu Y, Ye F. Photothermal Responsive Digital Polymerase Chain Reaction Resolving Exosomal microRNAs Expression in Liver Cancer. Small. 2023;19:e2207672
140. Boloix A, Feiner-Gracia N, Köber M, Repetto J, Pascarella R, Soriano A. et al. Engineering pH-Sensitive Stable Nanovesicles for Delivery of MicroRNA Therapeutics. Small. 2022;18:e2101959
141. Koustas E, Trifylli EM, Sarantis P, Papadopoulos N, Papanikolopoulos K, Aloizos G. et al. An Insight into the Arising Role of MicroRNAs in Hepatocellular Carcinoma: Future Diagnostic and Therapeutic Approaches. Int J Mol Sci. 2023;24:7168
142. Farzaneh Z, Vosough M, Agarwal T, Farzaneh M. Critical signaling pathways governing hepatocellular carcinoma behavior; small molecule-based approaches. Cancer Cell Int. 2021;21:208
143. Stasevich EM, Murashko MM, Zinevich LS, Demin DE, Schwartz AM. The Role of Non-Coding RNAs in the Regulation of the Proto-Oncogene MYC in Different Types of Cancer. Biomedicines. 2021;9:921
144. Li X, Wang X, Liu N, Wang Q, Hu J. Inhibition of Metastatic Hepatocarcinoma by Combined Chemotherapy with Silencing VEGF/VEGFR2 Genes through a GalNAc-Modified Integrated Therapeutic System. Molecules. 2022;27:2082
145. Santo D, Mendonça PV, Serra AC, Coelho JFJ, Faneca H. Targeted downregulation of MYC mediated by a highly efficient lactobionic acid-based glycoplex to enhance chemosensitivity in human hepatocellular carcinoma cells. Int J Pharm. 2023;637:122865
146. Tabernero J, Shapiro GI, LoRusso PM, Cervantes A, Schwartz GK, Weiss GJ. et al. First-in-humans trial of an RNA interference therapeutic targeting VEGF and KSP in cancer patients with liver involvement. Cancer Discov. 2013;3:406-17
147. Lee SJ, Yook S, Yhee JY, Yoon HY, Kim MG, Ku SH. et al. Co-delivery of VEGF and Bcl-2 dual-targeted siRNA polymer using a single nanoparticle for synergistic anti-cancer effects in vivo. J Control Release. 2015;220:631-41
148. Bakrania A, To J, Zheng G, Bhat M. Targeting Wnt-β-Catenin Signaling Pathway for Hepatocellular Carcinoma Nanomedicine. Gastro Hep Adv. 2023;2:948-63
149. Schneider P, Zhang H, Simic L, Dai Z, Schrörs B, Akilli-Öztürk Ö. et al. Multicompartment Polyion Complex Micelles Based on Triblock Polypept(o)ides Mediate Efficient siRNA Delivery to Cancer-Associated Fibroblasts for Antistromal Therapy of Hepatocellular Carcinoma. Adv Mater. 2024;36:e2404784
150. Luo R, Le H, Wu Q, Gong C. Nanoplatform-Based In Vivo Gene Delivery Systems for Cancer Therapy. Small. 2024;20:e2312153
151. Sun B, Wu W, Narasipura EA, Ma Y, Yu C, Fenton OS. et al. Engineering nanoparticle toolkits for mRNA delivery. Adv Drug Deliv Rev. 2023;200:115042
152. Zong Y, Lin Y, Wei T, Cheng Q. Lipid Nanoparticle (LNP) Enables mRNA Delivery for Cancer Therapy. Adv Mater. 2023;35:e202303261
153. Lai I, Swaminathan S, Baylot V, Mosley A, Dhanasekaran R, Gabay M. et al. Lipid nanoparticles that deliver IL-12 messenger RNA suppress tumorigenesis in MYC oncogene-driven hepatocellular carcinoma. J Immunother Cancer. 2018;6:125
154. Cheng Q, Tao W, Wei T. Lipid nanoparticles for mRNA therapy: recent advances in targeted delivery. Life Med. 2022;1:21-23
155. Cao J, Choi M, Guadagnin E, Soty M, Silva M, Verzieux V. et al. mRNA therapy restores euglycemia and prevents liver tumors in murine model of glycogen storage disease. Nat Commun. 2021;12:3090
156. Lei S, Chen X, Gao Y, Shuai M, Zhou W, Li J. et al. ALPPL2-binding peptide facilitates targeted mRNA delivery for efficient hepatocellular carcinoma gene therapy. Adv Funct Mater. 2022;32:2204342
157. Wang Y, Zhang Z, Luo J, Han X, Wei Y, Wei X. mRNA vaccine: a potential therapeutic strategy. Mol Cancer. 2021;20:33
158. Fu J, Chen F, Lin Y, Gao J, Chen A, Yang J. Discovery and characterization of tumor antigens in hepatocellular carcinoma for mRNA vaccine development. J Cancer Res Clin Oncol. 2023;149:4047-61
159. Tojjari A, Saeed A, Singh M, Cavalcante L, Sahin IH, Saeed A. A Comprehensive Review on Cancer Vaccines and Vaccine Strategies in Hepatocellular Carcinoma. Vaccines. 2023;11:1357
160. Wang HK, Xu XH, Wang SM, Zhang HY. Preparation of hepatocellular carcinoma mRNA vaccines based on potential tumor targets and immunophenotypes. Transl Cancer Res. 2024;13:173-90
161. Ho W, Gao M, Li F, Li Z, Zhang XQ, Xu X. Next-Generation Vaccines: Nanoparticle-Mediated DNA and mRNA Delivery. Adv Healthc Mater. 2021;10:e2001812
162. Voutila J, Reebye V, Roberts TC, Protopapa P, Andrikakou P, Blakey DC. et al. Development and Mechanism of Small Activating RNA Targeting CEBPA, a Novel Therapeutic in Clinical Trials for Liver Cancer. Mol Ther. 2017;25:2705-14
163. Sartorius K, Antwi SO, Chuturgoon A, Roberts LR, Kramvis A. RNA Therapeutic Options to Manage Aberrant Signaling Pathways in Hepatocellular Carcinoma: Dream or Reality? Front Oncol. 2022;12:891812
164. Zhao X, Reebye V, Hitchen P, Fan J, Jiang H, Saetrom P. et al. Mechanisms involved in the activation of C/EBPα by small activating RNA in hepatocellular carcinoma. Oncogene. 2019;38:3446-57
165. Huan H, Wen X, Chen X, Wu L, Liu W, Habib NA. et al. C/EBPα Short-Activating RNA Suppresses Metastasis of Hepatocellular Carcinoma through Inhibiting EGFR/β-Catenin Signaling Mediated EMT. PloS One. 2016;11:e0153117
166. Hui L, Zheng F, Bo Y, Sen-Lin M, Ai-Jun L, Wei-Ping Z. et al. MicroRNA let-7b inhibits cell proliferation via upregulation of p21 in hepatocellular carcinoma. Cell Biosci. 2020;10:83
167. Kosaka M, Kang MR, Yang G, Li LC. Targeted p21WAF1/CIP1 activation by RNAa inhibits hepatocellular carcinoma cells. Nucleic Acid Ther. 2012;22:335-43
168. Bi CQ, Kang T, Qian YK, Kang M, Zeng XH, Li LC. Upregulation of LHPP by saRNA inhibited hepatocellular cancer cell proliferation and xenograft tumor growth. PloS One. 2024;19:e0299522
169. Lau D, Bobe AM, Khan AA. RNA Sequencing of the Tumor Microenvironment in Precision Cancer Immuno-therapy. Trends Cancer. 2019;5:149-56
170. Ferdows BE, Patel DN, Chen W, Huang X, Kong N, Tao W. RNA cancer nanomedicine: nanotechnology-mediated RNA therapy. Nanoscale. 2022;14:4448-55
171. Zhan Q, Yi K, Qi H, Li S, Li X, Wang Q. et al. Engineering blood exosomes for tumor-targeting efficient gene/chemo combination therapy. Theranostics. 2020;10:7889-905
172. Kumar K, Rani V, Mishra M, Chawla R. New paradigm in combination therapy of siRNA with chemotherapeutic drugs for effective cancer therapy. Curr Res Pharmacol Drug Discov. 2022;3:100103
173. Lin YX, Wang Y, Ding J, Jiang A, Wang J, Yu M. et al. Reactivation of the tumor suppressor PTEN by mRNA nanoparticles enhances antitumor immunity in preclinical models. Sci Transl Med. 2021;13:eaba9772
174. de Melo Silva AJ, de Melo Gama JE, de Oliveira SA. The Role of Bcl-2 Family Proteins and Sorafenib Resistance in Hepatocellular Carcinoma. Int J Cell Biol. 2024;2024:4972523
175. Tang W, Chen Z, Zhang W, Cheng Y, Zhang B, Wu F. et al. The mechanisms of sorafenib resistance in hepatocellular carcinoma: theoretical basis and therapeutic aspects. Signal Transduct Target Ther. 2020;5:87
176. Lin G, Revia RA, Zhang M. Inorganic Nanomaterial-Mediated Gene Therapy in Combination with Other Antitumor Treatment Modalities. Adv Funct Mater. 2021;31:2007096
177. Jin H, Wang L, Bernards R. Rational combinations of targeted cancer therapies: background, advances and challenges. Nat Rev Drug Discov. 2023;22:213-34
178. Deng Z, Yang H, Tian Y, Liu Z, Sun F, Yang P. An OX40L mRNA vaccine inhibits the growth of hepatocellular carcinoma. Front Oncol. 2022;12:975408
179. Kumar V, Rahman M, Gahtori P, Al-Abbasi F, Anwar F, Kim HS. Current status and future directions of hepatocellular carcinoma-targeted nanoparticles and nanomedicine. Expert Opin Drug Deliv. 2021;18:673-94
180. Gu W, Meng F, Haag R, Zhong Z. Actively targeted nanomedicines for precision cancer therapy: Concept, construction, challenges and clinical translation. J Control Release. 2021;329:676-95
181. Liu Z, Wang S, Tapeinos C, Torrieri G, Känkänen V, El-Sayed N. et al. Non-viral nanoparticles for RNA interference: Principles of design and practical guidelines. Adv Drug Deliv Rev. 2021;174:576-612
182. Lu M, Huang Y. Bioinspired exosome-like therapeutics and delivery nanoplatforms. Biomaterials. 2020;242:119925
183. Shi Y, Zhen X, Zhang Y, Li Y, Koo S, Saiding Q. et al. Chemically Modified Platforms for Better RNA Therapeutics. Chem Rev. 2024;124:929-1033
184. Summer M, Ashraf R, Ali S, Bach H, Noor S, Noor Q. et al. Inflammatory response of nanoparticles: Mechanisms, consequences, and strategies for mitigation. Chemosphere. 2024;363:142826
185. Chen BQ, Zhao Y, Zhang Y, Pan YJ, Xia HY, Kankala RK. et al. Immune-regulating camouflaged nanoplatforms: A promising strategy to improve cancer nano-immunotherapy. Bioact Mater. 2023;21:1-19
186. Li B, Raji IO, Gordon AGR, Sun L, Raimondo TM, Oladimeji FA. et al. Accelerating ionizable lipid discovery for mRNA delivery using machine learning and combinatorial chemistry. Nat Mater. 2024;23:1002-8
187. Xu Y, Ma S, Cui H, Chen J, Xu S, Gong F. et al. AGILE platform: a deep learning powered approach to accelerate LNP development for mRNA delivery. Nature communications. 2024;15:6305
188. Craig AJ, von Felden J, Garcia-Lezana T, Sarcognato S, Villanueva A. Tumour evolution in hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2020;17:139-52
189. Lei Y, Tang R, Xu J, Wang W, Zhang B, Liu J. et al. Applications of single-cell sequencing in cancer research: progress and perspectives. J Hematol Oncol. 2021;14:91
190. Clark AJ, Lillard JW Jr. A Comprehensive Review of Bioinformatics Tools for Genomic Biomarker Discovery Driving Precision Oncology. Genes. 2024;15:1036
191. Ho D, Quake SR, McCabe ERB, Chng WJ, Chow EK, Ding X. et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020;38:497-518
192. Gatenby RA, Brown JS. Integrating evolutionary dynamics into cancer therapy. Nat Rev Clin Oncol. 2020;17:675-86
Author contact
![]() Corresponding authors: Xiong-Yongfuedu.cn (Y. Xiong), ORCID: 0000-0001-9016-8509; wing_young7com (Y. Yang), ORCID: 0000-0002-1090-3065; yzhang169harvard.edu (Y. Zhang), ORCID: 0000-0002-3476-8937.
Corresponding authors: Xiong-Yongfuedu.cn (Y. Xiong), ORCID: 0000-0001-9016-8509; wing_young7com (Y. Yang), ORCID: 0000-0002-1090-3065; yzhang169harvard.edu (Y. Zhang), ORCID: 0000-0002-3476-8937.
 Global reach, higher impact
Global reach, higher impact