13.3
Impact Factor
Theranostics 2025; 15(2):560-584. doi:10.7150/thno.103491 This issue Cite
Review
Silk fibroin-based hydrogels for cartilage organoids in osteoarthritis treatment
1. Institute of Translational Medicine, Shanghai University, Shanghai, 200444, China.
2. Organoid Research Center, Shanghai University, Shanghai, 200444, China.
3. National Center for Translational Medicine (Shanghai) SHU Branch, Shanghai University, Shanghai, 200444, China.
4. School of Medicine, Shanghai University, Shanghai, 200444, China.
5. Department of Orthopedics, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 200092, China.
6. Department of Anesthesiology, Shanghai Zhongye Hospital, Shanghai, 200941, China.
7. Department of Orthopedics, Honghui Hospital, Xi'an Jiao Tong University, Xi'an, 710000, China.
*These authors contributed equally to the work.
Received 2024-9-10; Accepted 2024-11-6; Published 2025-1-1
Abstract
Osteoarthritis (OA) is a common joint disease characterized by cartilage degeneration. It can cause severe pain, deformity and even amputation risk. However, existing clinical treatment methods for cartilage repair present certain deficiencies. Meanwhile, the repair effect of cartilage tissue engineering is also unsatisfactory. Cartilage organoids are multicellular aggregates with cartilage-like three-dimensional structure and function. On the one hand, cartilage organoids can be used to explore the pathogenesis of OA by constructing disease models. On the other hand, it can be used as filler for rapid cartilage repair. Extracellular matrix (ECM)-like three-dimensional environment is the key to construct cartilage organoids. Silk fibroin (SF)-based hydrogels not only have ECM-like structure, but also have unique mechanical properties and remarkable biocompatibility. Therefore, SF-based hydrogels are considered as ideal biomaterials for constructing cartilage organoids. In this review, we reviewed the studies of cartilage organoids and SF-based hydrogels. The advantages of SF-based hydrogels in constructing cartilage organoids and the iterative optimization of cartilage organoids through designing hydrogels by using artificial intelligence (AI) calculation are also discussed. This review aims to provide a theoretical basis for the treatment of OA using SF-based biomaterials and cartilage organoids.
Keywords: Osteoarthritis, Silk fibroin, Hydrogels, Cartilage organoids, Cartilage regeneration.
1. Introduction
Osteoarthritis (OA) is a joint disease characterized by cartilage degeneration [1-5]. Pathogenic factors of OA are mainly associated with obesity and age [6]. As the global aging and obese population rises, the number of OA patients will increase sharply in the next decade [7, 8]. Statistically, approximately 595 million people worldwide are affected by OA. And by 2050, the prevalence is projected to increase by over 200%, resulting in substantial economic burdens on both individuals and society [9]. Cartilage degeneration plays a significant role in the progression of OA, as it contributes not only to the disease outcome but also to its worsening [10, 11]. Therefore, repairing cartilage is a valuable strategy for the treatment and prevention of OA.
Cartilage has limited self-repair capacity [12-14]. As an immune-privileged tissue, it makes engineered cartilage analogs attractive candidates for off-the-shelf grafts in allogeneic transplantation. Organoids are simplified multicellular structures that develop from stem cells or organ progenitors through in vitro 3D culture combined with targeted induction technology, enabling the formation of organ-specific architectures and functions [15-17]. Specifically, cartilage organoids are tissues with cartilage structure, function, physiological and pathological characteristics through cultivating and assembling stem cells or chondrocytes [18, 19]. This offers a novel approach for cartilage regeneration. Compared to autologous chondrocyte implantation (ACI), cartilage organoid transplantation eliminates the need for a secondary surgery to harvest cells, streamlining the procedure and reducing postoperative complications. Techniques like ACI and matrix-induced autologous chondrocyte implantation (MACI), which rely on 2D chondrocyte expansion, are time-consuming and increase the risk of dedifferentiation into fibrocartilage [20-22]. In contrast, cartilage organoids have distinct advantages: they replicate the natural cartilage structure and can be directly implanted to repair defects, ensuring that the regenerated tissue closely resembles native cartilage. Furthermore, as they already mimic cartilage properties, cartilage organoids can seamlessly integrate with native tissue, minimizing the need for further regeneration post-implantation and thus enhancing the overall repair efficiency [23].
Organoid construction methods are broadly divided into scaffold-free self-organization and biomaterial-based co-cultivation. Scaffold-free self-organization allows mesenchymal stem cells (MSCs) to naturally form complex tissue structures. This method is straightforward and has a lower risk of contamination, but it struggles with achieving consistent organoid size and uniformity. On the other hand, biomaterial-assisted co-cultivation uses scaffolds like hydrogels to provide structural support, allowing precise control over the organoid architecture and customization of the environment. This makes it ideal for developing organoids with consistent and predictable properties. Currently, Matrigel is the most commonly used material for organoid construction. However, its undefined composition and batch-to-batch variability result in inconsistent mechanical strength, making it less reliable for precise experimental needs. Additionally, Matrigel lacks the flexibility for customization in specific organoid culture contexts [18, 24, 25]. Silk fibroin (SF) hydrogels, as a natural macromolecular material, offer several advantages over Matrigel, including a well-defined structure, controllable mechanical properties, and high customizability. These features make SF hydrogels more suitable for precise tissue engineering applications [26-30]. Moreover, SF's excellent processability allows it to be adapted to various processing methods and functional modifications, making it versatile for preparing different types of cartilage tissue engineering materials [31-33]. Furthermore, SF hydrogels have excellent printability, enabling their use in 3D bioprinting for advanced biofabrication techniques [34-36]. Therefore, SF-based hydrogel has a great prospect for cartilage regeneration and cartilage organoids construction [37].
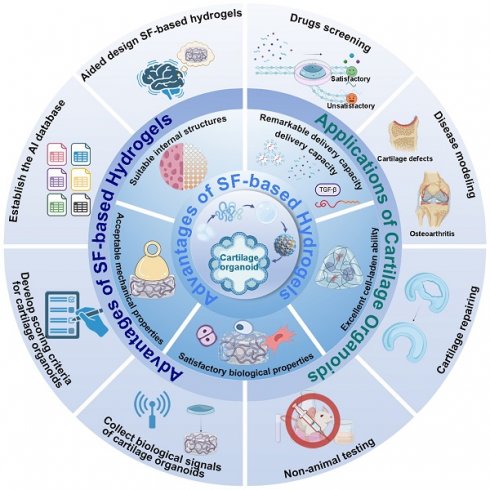
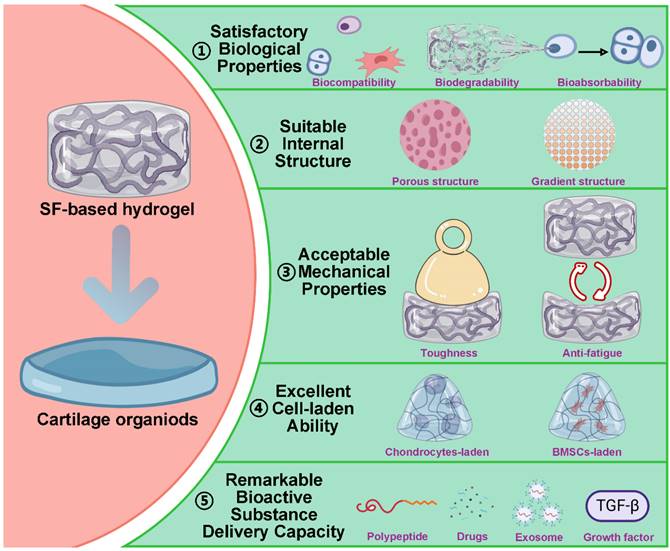
Herein, we summarize recent research on cartilage organoids and SF-based hydrogels, highlighting the advantages of SF-based hydrogels for cartilage organoid construction. The iterative optimization of cartilage organoids through designing hydrogels by using artificial intelligence (AI) calculation is also discussed (Figure 1). We hope that this review can provide a reference for cartilage organoids construction and a promising therapeutic strategy for OA.
2. Research progress in cartilage organoids
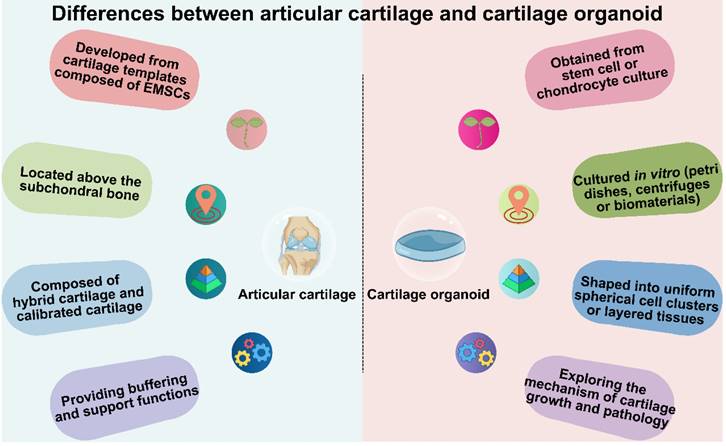
Cartilage is a critical component of the human body, providing essential support for mechanical reinforcement, cushioning, and protection (Figure 2). Cartilage development commences with a cartilaginous template constituted by embryonic mesenchymal stem cells. During this stage, primitive embryonic mesenchymal cells initiate differentiation into chondroblasts [38-40]. These chondroblasts proliferate and synthesize collagen fibers and glycosaminoglycans, establishing the extracellular matrix of cartilage. The distribution and orientation of collagen fibers and glycosaminoglycans, along with the degree of chondrocyte calcification, contribute to the multi-layered structure of cartilage. For example, articular cartilage can be broadly categorized into hyaline cartilage and calcified cartilage layers. Cartilage serves various physiological roles, with the most crucial being to provide cushioning and support within joints. It reduces friction between bones and protects them from wear and tear. Moreover, cartilage effectively disperses pressure generated during joint movement, thereby protecting joint tissues. In structures like the nose and ears, the elasticity and flexibility of cartilage allow it to maintain specific shapes [41, 42]. Currently, artificially engineered cartilage organoids structures are predominantly composed of uniformly spherical cell clusters or uniformly layered tissues. Research in cartilage organoids mainly focuses on understanding cartilage-related mechanisms, advancing plastic surgery, and promoting cartilage repair (Figure 3 and Figure 4).
Schematic diagram of SF-based hydrogels for construction of cartilage organoids. Created with BioRender.com.
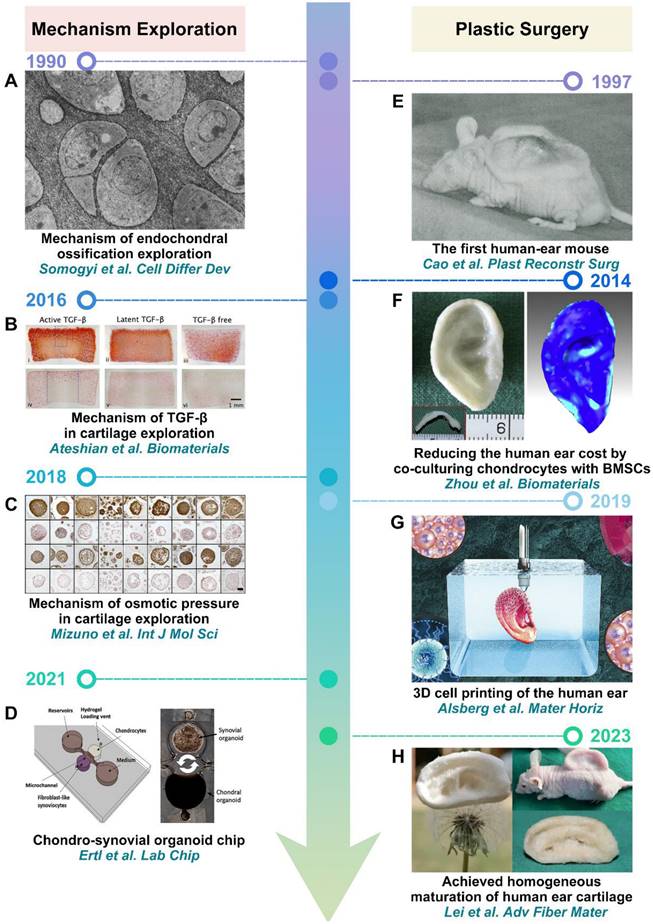
Cartilage organoids were initially applied to explore cartilage-related mechanisms. In 1990, Somogyi et al. pioneered the in vitro construction of cartilage organoids. By examining their morphology and ECM, they found that osteoblasts promoted mineralization within cartilage, whereas fibroblasts had inhibitory effects (Figure 3A) [43]. With the advancement of technology, cartilage organoids have also been utilized to investigate the impact of growth factors (TGF-β) and osmotic pressure on cartilage development (Figure 3B-C) [44, 45]. Furthermore, cartilage organoids have also been employed to construct organ-on-a-chip models to study inter-tissue interactions. For example, Ertl et al. constructed the chondro-synovial organoid chip to simulate cross-talk between individual synovial and cartilage organoids. Co-culturing with synovial organoids, it was demonstrated that cartilage organoids induced a heightened degree of cartilage physiology and structure, along with distinct cellular cytokine responses compared to their respective monocultures, underscoring the significance of inter-tissue cross-talk at the organ level in models of arthritic diseases (Figure 3D) [46]. In addition to exploring cartilage-related mechanisms, cartilage organoids have also demonstrated remarkable potential in plastic surgery. Notably, one of the most matured applications involves the construction of auricular-shaped cartilage organoids, particularly for reconstructing human ears [47]. In 1997, Cao et al. constructed the first human-ear mouse with a polyglycolic acid fiber scaffold (Figure 3E) [48]. Subsequently, Zhou et al. advanced the field by constructing human auricular cartilage organoids through co-culturing microtia chondrocytes and bone mesenchymal stem cells (BMSCs) (Figure 3F) [49]. This approach not only enhanced the shape stability of human auricular cartilage organoids but also effectively reduced construction costs. In 2019, Alsberg et al. further advanced the field by enhancing the shape resolution of human auricular cartilage organoids using 3D bioprinting technology (Figure 3G) [50]. Building on these advances, Lei et al. constructed homogeneous and mature human auricular cartilage organoids using synthetically engineered fiber-reinforced SF super elastic absorbent sponges (Figure 3H) [51].
Differences between articular cartilage and cartilage organoids in origin, location, structure, and function. Created with BioRender.com.
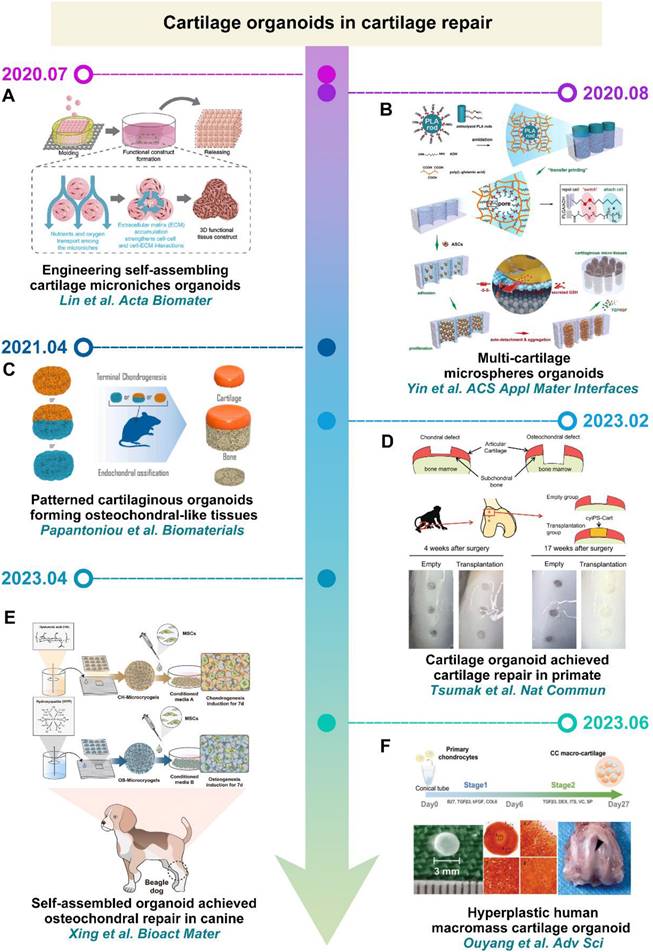
In recent years, researchers have increasingly directed their focus towards applying cartilage organoids in cartilage repair. For instance, Lin et al. and Yin et al. achieved the stacking of cartilage microsphere organoids using materials with self-assembling properties, enabling the construction of larger-volume cartilage organoids (Figure 4A-B) [52, 53]. Papantoniou et al. assembled cartilage microtissues derived from iPSC-derived chondrocytes with callus organoids (COs) sourced from human plasmacytoid dendritic cells to constructed layered osteochondral organoids (Figure 4C) [54]. It is worth noting that cartilage organoids constructed by Tsumaki et al. and Xing et al. successfully achieved cartilage repair in primates and canids (Figure 4D-E) [55, 56]. In addition, Ouyang et al. constructed macromass cartilage organoids up to 3 mm in diameter by culturing human polydactyly chondrocytes in customized culture, which can be used as implants to facilitate cartilage defect repair (Figure 4F) [57]. Based on these studies, it is evident that constructing cartilage organoids requires providing material support for seed cells and directing their chondrogenic differentiation. Consequently, to construct cartilage organoids that closely mimic the natural cartilage structure and function, novel smart biomaterials need to be designed to furnish the chondrogenic microenvironment necessary for seed cells.
3. Preparation of silk fibroin-based hydrogel
3.1. Characteristics of silk fibroin
SF is a naturally occurring macromolecular material produced by a range of animals, including silkworms, spiders, scorpions, mites, and flies [58]. It is worth noting that SF of different origins has obvious differences in structure and properties. Among them, silkworms-derived SF has been widely studied and applied in the clinic because of its unique mechanical properties and abundant yield [59, 60]. Hence, this review only discusses the silkworms derived SF. A single silk filament is composed of two strands of SF, enveloped in sericin (Figure 5A) [61].
The molecular structure of SF is very complex, which is composed of disulfide-linked heavy chain and light chain (Figure 5B). The heavy chain includes non-repetitive C-terminal and N-terminal, along with 11 hydrophilic segments composed of 31 amino acid residues and 12 hydrophobic segments. The hydrophobic segments mainly contain Gly-X repeats, where X can be Ala (65%), Ser (23%), or Tyr (9%). Repeated sequences include Gly-Ala-Gly-Ala-Gly-Ser (GAGAGS), Gly-Ala-Gly-Ala-Gly-Tyr (GAGAGY), and Gly-Ala-Gly-Ala-Gly-Ser-Gly-Ala-Ala-Ser (GAGAGSGAAS). These repetitive sequences can form crystalline β-sheet structures through hydrophobic interactions (Figure 5C) [26]. Contrary to the heavy chain, the amino acid sequence of the light chain is disordered and tends to form an amorphous structure [62]. Recent studies have revealed that SF achieves interfacial self-assembly due to its amphiphilic molecular structure, which promotes the formation of β-sheets at interfaces. This property is particularly useful in hydrogel formation, as the conformation of SF can be modulated by adjusting the water-to-organic phase ratio. These adjustments enable the creation of hydrogels specifically optimized for cartilage regeneration, offering enhanced mechanical properties and bioactivity for improved tissue repair [63].
Cartilage organoids in mechanism exploration and plastic surgery: (A) Reproduced with permission from ref [43]; Copyright 1990, Elsevier. (B) Reproduced with permission from ref [44]; Copyright 2016, Elsevier. (C) Reproduced with permission from ref [45]; Copyright 2018, MDPI. (D) Reproduced with permission from ref [46]; Copyright 2021, Royal Society of Chemistry. (E) Reproduced with permission from ref [48]; Copyright 1997, Wolters Kluwer Health, Inc. (F) Reproduced with permission from ref [49]; Copyright 2014, Elsevier. (G) Reproduced with permission from ref [50]; Copyright 2019, Royal Society of Chemistry. (H) Reproduced with permission from ref [51]; Copyright 2023, Springer Nature.
Cartilage organoids in tissue engineering: (A) Reproduced with permission from ref [52]; Copyright 2020, Elsevier. (B) Reproduced with permission from ref [53]; Copyright 2020, American Chemical Society. (C) Reproduced with permission from ref [54]; Copyright 2021, Elsevier. (D) Reproduced with permission from ref [55]; Copyright 2023, Springer Nature. (E) Reproduced with permission from ref [56]; Copyright 2023, Elsevier. (F) Reproduced with permission from ref [57]; Copyright 2023, Wiley-VCH GmbH.
SF exhibits exceptional physical and chemical properties due to its unique structure and composition. It can adopt four distinct conformations—silk I, silk II, silk III, and an amorphous structure—through intra- and intermolecular interactions. Among these, the amorphous structure and β-sheet-rich silk II conformation endow SF with high mechanical strength and toughness. Furthermore, silk I, silk II, silk III and amorphous structures can be transformed into each other by external effects (temperature, ultrasound, electric field, shear force and pH value) [62]. This adaptability makes SF highly suitable for diverse tissue regeneration applications, as its mechanical properties can be finely tuned. As a macromolecular protein material, SF also offers excellent cytocompatibility and biodegradability. It degrades in response to multiple proteases, with its degradation rate primarily controlled by the content of silk II. The degradation products—amino acids and peptides—are non-toxic and can be absorbed by cells, providing essential building blocks for tissue regeneration [76]. In addition to these favorable properties, SF's processability allows it to be adapted into various processing methods to meet the complex demands of tissue repair [77]. To provide a clearer understanding of SF's properties relative to other biomaterials commonly used in cartilage regeneration, Table 1 presents a quantitative comparison of SF with collagen, alginate, hyaluronic acid (HA), and Matrigel across key parameters, including mechanical properties, degradation rates, and biological performance.
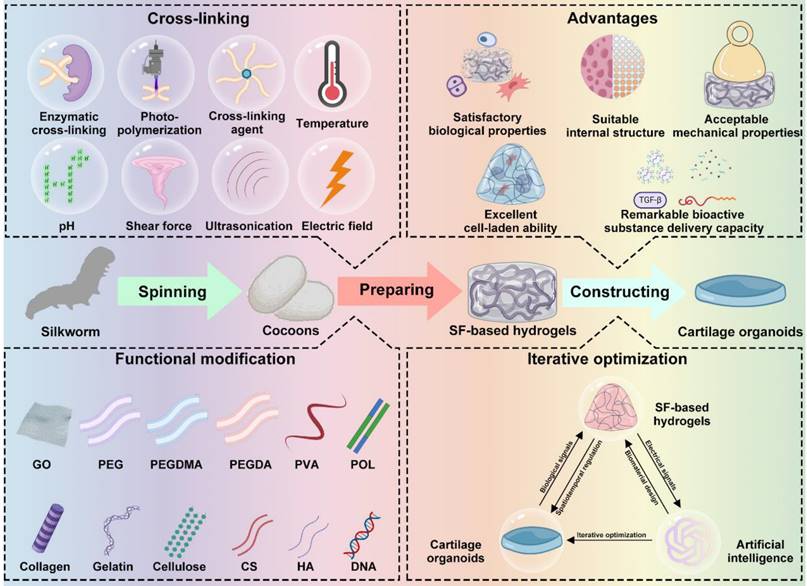
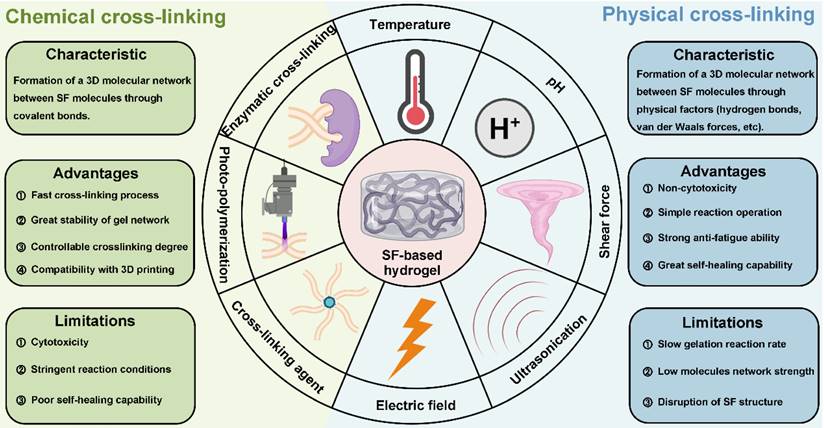
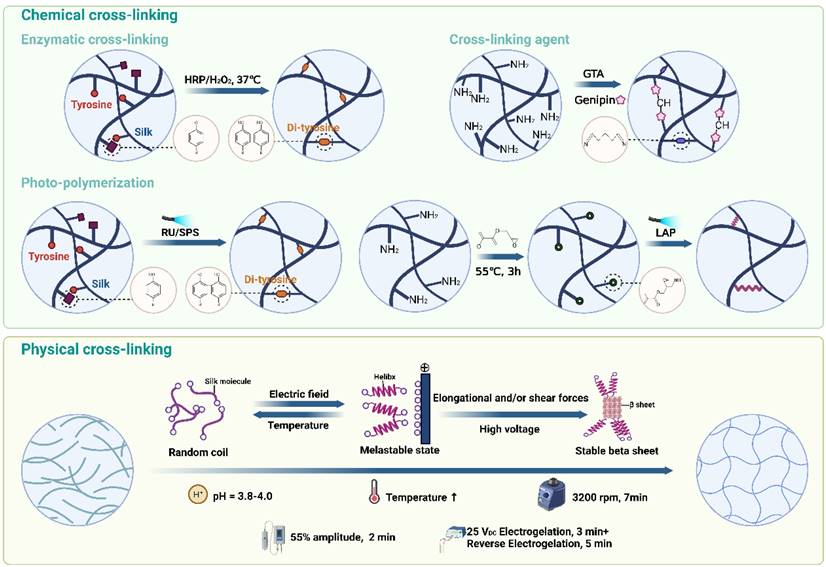
3.2. Cross-linking methods for silk fibroin-based hydrogels preparation
As previously mentioned, SF can be processed using various methods, including hydrogel preparation through cross-linking. Cross-linking methods are generally categorized into chemical and physical approaches [78]. Chemical cross-linking promotes the formation of covalent bonds by adding enzymes, cross-linking agents and photo-initiators to accelerate SF gelation. In contrast, physical cross-linking involves the self-assembly of SF into hydrogels by regulating physical parameters such as temperature, pH, shear force, ultrasound, and electric fields, each method offering distinct advantages and limitations (Figure 6, Table 2). The schematic in Figure 7 provides an overview of the mechanisms and preparation techniques employed in these cross-linking strategies for SF hydrogels.
3.2.1. Chemical cross-linking
Enzymatic cross-linking
In recent years, enzyme cross-linked hydrogels have attracted wide attention in the biomedicine field. For SF-based hydrogels, enzymes facilitate the formation of intermolecular covalent bonds by activating functional groups within SF. Additionally, enzymatic cross-linking induces the formation of an ECM-like elastic structure by controlling β-sheet formation, resulting in hydrogels with stable structures, controllable mechanical properties, and non-toxic effects on cells [79]. This method also supports cell encapsulation due to its cross-linking process being conducted at physiological pH and temperature [80].
Among the numerous enzymatic cross-linking reactions, horseradish peroxidase (HRP) mediated enzymatic cross-linking reaction is the most commonly used [81, 82]. It has the advantages of high selectivity, mild reaction conditions and no toxic components [83, 84]. HRP is typically combined with H2O2 to induce SF cross-linking by oxidizing tyrosine residues into o-quinone residues. These o-quinone residues then react with phenol or aniline to form covalent bonds, leading to intermolecular or intramolecular cross-linking [85]. For example, Hasturk et al. prepared SF/tyramine-substituted SF (SF-TA) composite hydrogel by using HRP and H2O2 [86]. The composite hydrogel exhibited adjustable mechanical properties, degradability, and excellent cytocompatibility, making it promising for cartilage defect repair due to its cell encapsulation capability. Li et al. further developed an SF-gelatin (SF-GT) hydrogel with a macroporous structure using HRP/H2O2 in combination with 3D bioprinting [87]. SF-GT hydrogel had structural stability, mechanical properties and adjustable degradation rate for cartilage reconstruction. Additionally, SF-GT hydrogel could induce stem cells to synthesize Col II at a higher level and show hyaline cartilage phenotype.
Comparison of the mechanical properties, degradation, cell viability, and chondrocyte differentiation of SF and other biomaterials used in cartilage tissue engineering.
| Property | SF | Col | Alginate | HA | Matrigel |
|---|---|---|---|---|---|
| Young's Modulus (MPa) | 300-700 MPa | 0.1-10 MPa | 0.01-1.5 MPa | 0.01-0.1 MPa | 0.00004-0.00045 MPa |
| Breaking Elongation (%) | 4%-26% | 10-30% | 10-20% | 5-20% | Not reported |
| Toughness (MJ/m3) | 70-78 MJ/m3 | 1-5 MJ/m³ | 1-5 MJ/m³ | 1-2 MJ/m³ | Not reported |
| Degradation Time | Tunable (weeks to months) | Days to weeks | Days to weeks | Days to weeks | Within a few days |
| Cell Viability (%) | >90% | >80% | >80% | >85% | >90% |
| Chondrocyte Differentiation | Supports viability and promotes collagen type II synthesis | Promotes moderate chondrocyte differentiation but limited stable phenotype | Supports chondrocyte viability with moderate differentiation capacity | Supports viability, requires additional cues for stable phenotype | Supports growth but does not inherently promote chondrocyte differentiation |
| References | [64, 65] | [66, 67] | [68-70] | [71, 72] | [73-75] |
Cross-linking methods for SF-based hydrogels: advantages and limitations.
| Type | Cross-linking Method | Advantages | Limitations |
|---|---|---|---|
| Chemical cross-linking | Enzymatic cross-linking | High selectivity; biocompatibility; tunable properties | High cost; low reaction velocity; limited scalability |
| Photo-polymerization | Rapid cross-linking; precise control | Potential cytotoxicity; limited tissue penetration | |
| Cross-linking agents | Cost-effective; enhances mechanical properties | Non-specific reactions; cytotoxicity (for some agents) | |
| Physical cross-linking | Temperature | Non-toxic; simple process | Lacks precision; risk of denaturation at high temperatures |
| pH | Effective control over gelation | Requires careful pH control; potential impact on cell viability | |
| Shear force | Creates directional structures; anisotropic properties | Requires specialized equipment; limited scalability | |
| Ultrasonication | Non-toxic; controllable process; tailored porosity | Weaker mechanical properties; limited load-bearing capacity | |
| Electric field | Enables gradient structures; useful for tissue engineering | Requires specialized equipment; potential for uneven cross-linking |
Source and structure of SF: (A) SF can be extracted from cocoon of silkworm. (B) SF molecule is composed of heavy chain and light chain connected by disulfide bond. (C) Crystal structure consists of GAGAGS, GAGAGY and GAGAGSGAAS repetitive sequences. Created with BioRender.com.
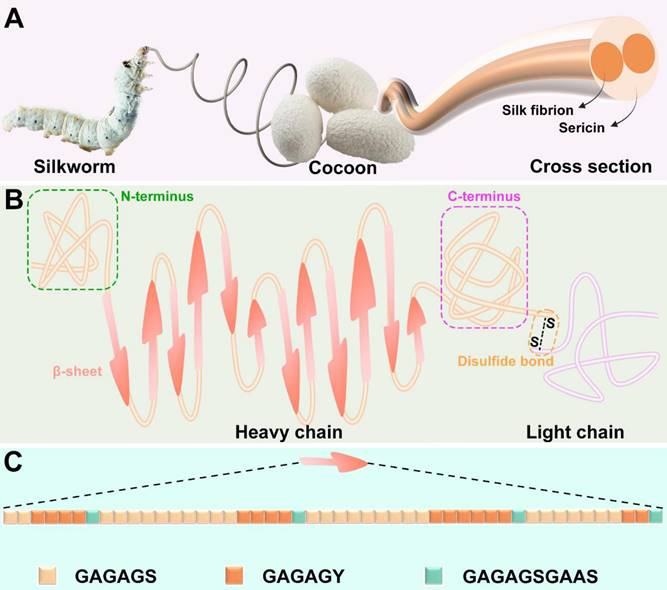
Photo-polymerization
Photo-polymerization is a widely used chemical cross-linking method that utilizes a photo-initiator and light (ultraviolet, visible, or gamma rays) to control the cross-linking process [88]. During photo-polymerization, the photo-initiator absorbs light energy and cleaves to produce free radicals, which subsequently react with unsaturated bonds in SF to induce cross-linking. The primary advantage of photo-polymerization is its extremely rapid cross-linking rate [89, 90]. For instance, Cui et al. successfully cross-linked SF within 1 minute using tris(2,2-bipyridyl)dichlororuthenium(II) hexahydrate and sodium persulfate as photo-initiators [91]. The SF-based hydrogels had stable mechanical properties and supported the long-term culture of human articular chondrocytes and cartilage tissue regeneration. In addition, there is a special photo-polymerization method using high-intensity gamma-ray without adding photo-initiators. This method can completely remove the toxic effects caused by photo-initiators residues [92]. For example, Kim et al. prepared chemically cross-linked SF hydrogels by using Co-60 derived gamma-ray (SF C-gel) [93]. They found that SF C-gel was biocompatible and could promote the attachment and proliferation of hMSCs.
Cross-linking agents
Cross-linking agent molecules can accelerate SF cross-linking by reacting with reactive groups such as -OH, -NH2 and -COOH in SF [94]. Compared to enzymes and photo-initiators, cross-linking agents are more cost-effective and can improve the mechanical properties of hydrogels [59]. Glutaraldehyde (GTA) is the most widely used cross-linking agent, which can promote SF cross-linking by reacting with the phenolic group of tyrosine. For instance, Srisawasdi et al. prepared polycarbazole/SF (SF/PCZ) hydrogels with glutaraldehyde as cross-linking agent [95]. They found that SF/PCZ hydrogel had good dielectric properties and excellent toughness. However, the biotoxicity of GTA limits its applications in tissue engineering and medicine. In contrast, genipin is a promising natural small molecule cross-linking agent due to its excellent biocompatibility. Considering this, Min et al. designed chitosan/SF hydrogels loaded with kartogenin (KGN) and platelet-derived growth factor BB (PDGF-BB) by using genipin as cross-linking agent [96]. The hydrogels allowed for the sustained release of KGN and PDGF-BB, supporting the growth of seed chondrocytes and maintaining their phenotype, demonstrating potential in cartilage tissue engineering.
3.2.2. Physical cross-linking
Temperature
Temperature significantly affects the cross-linking of proteins, including SF [97]. Increasing the temperature can promote SF cross-linking by enhancing the Brownian motion of SF molecules and increasing the effective collision rate between them. Additionally, elevated temperatures can disrupt the free energy state of SF molecules, exposing internal hydrophobic regions and facilitating the transition from random coil to β-sheet structures, thereby enhancing hydrophobic interactions and accelerating cross-linking [98]. For instance, Kim et al. researched the effect of cross-linking temperature for SF hydrogels [99]. They found that the cross-linking rate and compressive modulus of SF hydrogels increased with increasing cross-linking temperature within a certain range.
pH
In addition to temperature, the pH of the SF solution is also a critical factor in SF cross-linking. When the pH of the solution approaches the isoelectric point of SF (pH = 3.8-4.0), the electrostatic repulsion between SF molecules is minimized, making the molecules more prone to aggregation and cross-linking [94]. In this condition, the SF molecules are unstable and prone to aggregation and cross-linking. Therefore, adjusting the pH value of the solution is an effective method to induce SF cross-linking. For example, Nagarkar et al. investigated SF cross-linking by changing pH via adding HCl [100]. They found that adjusting the solution pH from 8 to 2 could prepare weak SF hydrogels. Additionally, Fini et al. designed and developed SF-based hydrogel though regulating pH via adding citric acid to SF solution [101]. They found that the hydrogel had good mechanical properties and excellent cytocompatibility. Additionally, in vivo experiments demonstrated that the hydrogel showed non-inflammatory response after implantation and stimulated cells to produce TGF-β1 to induce tissue regeneration.
Shear force
The shear force cross-linking method typically involves high-speed vortex treatment on SF solution [102]. High-speed vortex treatment accelerates β-sheet generation by stretching SF molecules and changing their orientation to promote SF cross-linking [103]. Moreover, this method can also be used to prepare SF-based hydrogels with directional structures. For example, Chen et al. fabricated SF/sodium surfactin hydrogels with directional three-dimensional structure by vortex treatment [104]. The hydrogel could accelerate 3D directed tissue regeneration due to its excellent anisotropy. Moreover, Kasoju et al. fabricated SF hydrogel with good mechanical properties by combining methanol treatment and vortex treatment [105]. These hydrogels demonstrated effective cell encapsulation and controlled drug release capabilities.
Ultrasonication
Ultrasonication is a physical cross-linking method commonly used to prepare SF hydrogels. The effect of this method is similar to the anterior silk gland of silkworm, which promotes SF cross-linking through local temperature increase and shear force [106]. This method is highly stable and controllable, as it allows for adjustments in output energy and duration. Importantly, it effectively avoids the toxicity issues associated with additives like photo-initiators and cross-linking agents [107]. For example, Byram et al. designed and developed SF/xanthan gum hydrogels by ultrasonication [108]. Additionally, due to their cartilage ECM-like microstructure, these hydrogels showed potential for applications in cartilage tissue engineering.
Electric field
As we mentioned before, SF is negatively charged in neutral solutions due to its isoelectric point (pH=3.8-4.0). Under an electric field, SF molecules aggregate near the anode, forming micelles that subsequently assemble into hydrogels through physical entanglement of molecular chains [109]. For instance, Liu et al. constructed SF electrogels with excellent mechanical properties via a low-voltage electric field [110]. They found that the hydrogel had excellent biocompatibility and drug loading capacity. In addition, gradient structure hydrogels which are more suitable for cartilage repair can be prepared by the electric field. Consider this, Xu et al. developed multi-functional beta-sheet rich silk nanofibers (BSNF) hydrogels with adjustable gradient mechanical strength and structure in electric field [111]. BSNF hydrogel could regulate BMSCs to differentiate into chondrocytes to promote cartilage repair due to its gradients structure.
3.3. Functional modifications
As we mentioned in 3.1. Characteristics of silk fibroin, SF has excellent biocompatibility, biodegradability and mechanical properties. However, after various physical and chemical treatments, the molecular structure of SF is destroyed, which leads to the unsatisfactory mechanical strength of pure SF hydrogel. In addition, pure SF hydrogel has certain disadvantages, such as insufficient water retention, poor antibacterial properties and unsatisfactory cartilage repair properties [138]. In order to improve SF hydrogel, it is an effective strategy to prepare composite SF hydrogel by mixing some functional materials into SF solution [139]. These functional materials can be divided into synthetic materials and natural materials (Table 3).
3.3.1. Synthetic material modification
Graphene oxide is a kind of functional carbon allotrope. Recently, it has attracted increasing attention in the field of materials due to its excellent mechanical strength, attractive surface volume ratio, high water solubility, easy solution processing and chemical functionality [140]. The incorporation of GO into SF solutions can significantly enhance the mechanical properties of SF-based hydrogels. For example, Wang et al. developed nano-hydroxyapatite-GO/SF hydrogels using click chemistry, resulting in enhanced mechanical strength compared to pure SF hydrogels, with a compressive modulus of 95.4 ± 2.0 kPa [112]. Furthermore, the addition of GO can improve the toughness of SF hydrogels. Balu et al. fabricated regenerated SF (RSF)/GO nanocomposite hydrogels using RuBPY as a photo-initiator, achieving mechanical properties superior to natural cartilage, with a Young's modulus of 8 MPa and tensile toughness of 2.4 MJ/m3 [113].
Cross-linking methods of SF-based hydrogels. Chemical cross-linking: enzymatic cross-linking, photo-polymerization and cross-linking agent. Physical cross-linking: temperature, pH, shear force ultrasonication and electric field. Created with BioRender.com.
The functional materials that have been used in combination with SF to prepare composite hydrogels for cartilage repair.
| Type | Functional materials | Preparation method | Advantages of composite hydrogels in cartilage repair | References |
|---|---|---|---|---|
| Synthetic | GO | Photo-polymerization with RuBPY as photo-initiators | Excellent mechanical properties | [112, 113] |
| PEG | Ultrasonication | Injectable; rapid gelation; suitable microenvironment | [114] | |
| PEGDMA | UV photo-polymerization | Adjustable mechanical properties | [115] | |
| PEGDA | Photo-polymerization with LAP as photo-initiators | Excellent mechanical properties; bioprinting-compatible | [116] | |
| poly(N-vinylcaprolactam) | Photo-polymerization with tris(2,2-bipyridyl)dichlororuthenium(II) and ammonium peroxodisulfate as photo-initiators | Enhanced water uptake capacity, elasticity and toughness | [117] | |
| PVA | pH adjustment | Excellent mechanical properties; high porosity; adjustable swelling ratio | [118] | |
| POL | Enzyme cross-linking catalyzed by HRP and H2O2 | Thermosensitive; injectable | [119, 120] | |
| MXene | Enzyme cross-linking catalyzed by HRP and H2O2; Ultrasound technique | Metallic conductivity; piezoelectricity; excellent hydrophilicity; diverse surface chemical properties; injectable | [121, 122] | |
| Natural | Collagen | Ultrasonication | Promotes MSC proliferation; chondrogenic differentiation | [123, 124] |
| Gelatin | Enzyme cross-linking catalyzed by transglutaminase | Cell attachment, proliferation; excellent mechanical integrity | [125, 126] | |
| HPMC | Heating | Excellent mechanical properties | [127] | |
| CS | Enzyme cross-linking catalyzed by HRP and H2O2 | Environmentally sensitive; controlled release of drugs and growth factors | [128-131] | |
| HA | Enzyme cross-linking catalyzed by HRP and H2O2 | MSC recruitment; cell adhesion; cartilage-like mechanical properties | [132-135] | |
| GA | Photo-polymerization | Reduced mechanical stress; lower in vivo friction coefficients | [136] | |
| DNA | Enzyme cross-linking catalyzed by HRP and H2O2 and complementary base pairing | Regulate chondrogenic differentiation of BMSCs | [137] |
Synthetic polymers are also commonly used to prepare composite hydrogels. Among them, polyethylene glycol (PEG) has received wide attention due to its versatility in molecular weight, topology (linear, branched, star-shaped) [139, 141]. Interestingly, the incorporation of PEG can endow the SF composite hydrogel with the injectable property. For example, Zhang et al. prepared injectable BMSC-encapsulated dual-network SF-PEG composite hydrogels via ultrasonication, resulting in hydrogels with a high cross-linking rate, excellent biocompatibility, and strong mechanical strength. Additionally, these dual-network SF-PEG hydrogels promoted cartilage repair by enhancing BMSC chondrogenic differentiation [114]. Furthermore, derivatives of PEG can also strengthen the cartilage repair ability of SF hydrogels. For instance, Achachelouei et al. fabricated SF/poly(ethylene glycol) dimethacrylate (PEGDMA) hydrogels with adjustable mechanical properties by photo-polymerization [115]. They found that the compression modulus of SF/PEGDMA hydrogel was related to the ratio of SF to PEGDMA. Meanwhile, Bandyopadhyay et al. constructed silk methacrylate (SilMA)-PEG diacrylate hydrogel with excellent mechanical properties and adjustable degradability via photo-polymerization [116]. Importantly, this hydrogel was suitable for chondrocytes-laden 3D biological printing to accelerate cartilage repair.
Apart from PEG, the performance of SF hydrogels can be enhanced by mixing with poly(N-vinylcaprolactam), poly vinyl alcohol, poloxamer [142]. For instance, Whittaker et al. constructed RSF-poly(N-vinylcaprolactam) double network (DN) hydrogel by a rapid one-pot method [117]. Compared with SF hydrogels, poly(N-vinylcaprolactam) enhanced elasticity and toughness of hybrid hydrogels. Furthermore, Subramanian et al. developed Mo3Se3-PVA-SF nanowire hydrogel with remarkable mechanical properties by using glutaraldehyde as cross-linking agent [118]. They found the composite could stimulate the expression of collagen to accelerate tissue repair. It is worth noting that POL can impart injectability to SF hydrogel [120]. For example, Min et al. constructed an injectable alginate-poloxamer (ALG-POL)/SF hydrogel though using HRP and H2O2 [119]. The injectability of this hydrogel was attributed to its solution-gel transition properties at physiological temperature. In addition, ALG-POL/SF hydrogel accelerated cartilage regeneration by promoting chondrocyte proliferation.
MXenes, as novel 2D nanomaterials composed of transition metal complexes, had been applied in biomedicine due to their metallic conductivity, piezoelectricity, excellent hydrophilicity, and diverse surface chemical properties. Jiang et al. utilized enzyme crosslinking to combine MXene nanosheets with SF, forming a piezoresistive nanocomposite hydrogel that facilitated bone tissue regeneration by restoring the electrical microenvironment [121]. Additionally, Yang et al. developed an injectable SF/MXene conductive hydrogel developed through ultrasound techniques, which acted as a stem cell carrier and enabled in vivo electrical stimulation for repairing brain tissue damage [122].
3.3.2. Natural material modification
The mixing of synthetic materials in SF hydrogels may introduce cytotoxicity. Conversely, the combination of SF with natural materials can avoid the toxicity problems associated with synthetic materials [143]. Currently, composite hydrogels have been prepared by combining with GT, collagen, cellulose or HA [144, 145].
Collagen (Col) is the most abundant natural polymer in ECM with remarkable biocompatibility, negligible immunogenicity and strong biological activity. Notably, collagen can enhance cartilage regeneration effects as it promotes the attachment and chondrogenic differentiation of MSCs [123]. For example, Zhang et al. developed an injectable BMSC-laden collagen-PEG/SF DN hydrogel via ultrasonication, which exhibited enhanced mechanical strength and cytocompatibility, ultimately accelerating cartilage regeneration [124].
GT is a mixture of large polypeptides, denatured from collagen. GT is a promising material in tissue engineering attributed to its high swelling and thermal inversion properties [125]. In addition, GT can form an interpenetrating network (IPN) with SF to enhance the compressive moduli of SF-based hydrogel. Park et al. fabricated GT-SF IPN hydrogels through microbial transglutaminase-induced cross-linking, resulting in biodegradable, non-cytotoxic hydrogels with superior mechanical properties compared to individual GT or SF hydrogels. The resulting composite hydrogel also promoted cell adhesion and proliferation [126].
Cellulose is a polysaccharide biomolecular material available in various sources [146-148]. Noticeably, cellulose can be modified in several ways to generate cellulose derivatives [149]. These cellulose derivatives strengthen the compressive modulus of SF-based hydrogels by inducing the generation of β-sheets. For instance, Luo et al. fabricated RSF/hydroxypropyl methyl cellulose (HPMC) hydrogel with excellent mechanical properties [127]. The maximum compressive and tensile modulus of this hydrogel exceeded 1.0 MPa.
Schematic representation of the mechanisms and preparation methods of different cross-linking approaches for SF-based hydrogels. Created with BioRender.com.
Chitosan (CS) is a kind of polysaccharide biopolymer, which has an inherent linear structure, excellent biocompatibility and environmental responsiveness. It has been proved that SF hydrogels can be endowed with environmental responsiveness by combining with CS [128]. For example, Xu et al. developed pH responsiveness SF/CS hydrogel by chemical cross-linking [129]. Meanwhile, Yu et al. prepared CS/SF/amino-functionalized mesoporous silica hydrogel through using genipin as cross-linking agent [130]. They found that the excellent injectability of the composite hydrogel was due to its sensitive thermal responsiveness at physiological pH. Additionally, CS-SF composite hydrogels can achieve controlled drug release. Dong et al. prepared a p-hydroxybenzene propanoic acid-modified chitosan (PC)/SF hydrogel using an HRP-mediated enzymatic cross-linking reaction, which sequentially released bioactive molecules to induce MSC homing and chondrogenic differentiation [131].
HA is a common biodegradable, non-immunogenic and non-inflammatory polysaccharide in the human body. It has been reported that mixing HA can enhance the storage modulus and compressive modulus of SF hydrogels [132, 150]. For example, Ziadlou et al. designed and developed HA-TA /SF composite hydrogels via enzymatic cross-linking [133]. Compared with pure SF hydrogel, they found this hybrid hydrogel had enhanced storage modulus and drug releasing ability to stimulate cartilage regeneration, remarkable mechanical properties and drug release ability. Moreover, Wang et al. also fabricated an SF-HA composite hydrogel scaffold by combining SF/HA-Tyr hydrogel with SF sponge, finding that this biomaterial accelerated cartilage repair due to its excellent mechanical properties and MSC recruitment ability [134]. Fan et al. compounded SF with aldehyde-HA to create a dynamic network that delayed or interrupted the β-sheet-induced hardening of SF chains, producing a hydrogel matrix with mechanical properties similar to biological tissues [135].
Glycyrrhizic acid (GA), a natural compound from licorice roots, effectively inhibits intrinsic inflammation and, when combined with SF, modifies the mechanical properties of materials to reduce mechanical stress and lower friction coefficients in vivo after implantation. Zhang et al. developed a nanocomposite hydrogel for spinal cord repair by creating an interpenetrating polymer network with self-assembled GA as the first network and photo-crosslinked SilMA as the second network [136].
Deoxyribonucleic acid (DNA) is a natural macromolecular material, and hydrogels prepared using DNA exhibit unique programmability, good injectability, controllable mechanical properties, and are adaptable for 3D cell printing [17]. It has been demonstrated that DNA hydrogels have significant potential in protecting seed cells, particularly in the field of cartilage repair [151]. Recently, our team introduced DNA into SF hydrogels, imparting them with controllable surface rigidity to regulate the chondrogenic differentiation of BMSCs, thereby achieving a breakthrough in cartilage repair [137]. Details will be discussed in 4.3. Acceptable mechanical properties.
4. Advantages of silk fibroin-based hydrogels in the construction of cartilage organoids
Based on multiple cross-linking and modifications strategy, SF-based hydrogels have great potential in promoting cartilage regeneration [152]. Meanwhile, it also demonstrates that SF-based hydrogels have certain advantages in constructing cartilage organoids, including: satisfactory biological properties, suitable internal structure, acceptable mechanical properties, excellent cell-laden ability and remarkable bioactive substance delivery capacity (Figure 8).
4.1. Satisfactory biological properties
An ideal hydrogel for constructing cartilage organoids is inadmissible to inhibit the normal metabolic activity of cells, cause inflammatory responses, or induce apoptosis. For pure SF hydrogels, the problem of immunogenicity can be avoided by degumming completely. For SF-based composite hydrogels, the additional materials should have excellent biocompatibility and biodegradability. In addition, the construction of cartilage organoids is a dynamic and continuous process. Therefore, the SF hydrogel applied to the construction of cartilage organoids should have an appropriate degradation rate [153]. During the construction of cartilage organoids, SF hydrogels should be degraded gradually to reserve space for newborn cartilage tissue. Furthermore, all the degradation products of SF hydrogel are non-cytotoxic and can be absorbed by cells to provide a nutritional basis for cartilage regeneration [65].
4.2. Suitable internal structure
SF-based hydrogels can mimic the ECM of cartilage due to their hydrophilic three-dimensional porous structure [91]. As a substitute for ECM, the porous structure of SF-based hydrogel can provide channels for the diffusion of nutrients into chondrocytes, the migration of chondrocytes and the removal of metabolic waste [87, 154, 155]. It is worth noting that the extracellular matrix of cartilage is heterogeneous. From outside to inside, cartilage tissue can be divided into superficial zone, middle zone, deep zone and calcified zone. The composition and content of ECM are different in each zone [156]. Therefore, the ideal SF hydrogel for constructing cartilage organoids should have a multi-level or a gradient structure. For instance, Guo et al. fabricated SF/R5 peptide composite hydrogel with gradient structure [157]. The hydrogel could regulate the differentiation of BMSCs and accelerate cartilage repair.
Advantages of SF-based hydrogels in the construction of cartilage organoids: satisfactory biological properties, suitable internal structure, acceptable mechanical properties, excellent cell-laden ability and remarkable bioactive substance delivery capacity. Created with BioRender.com.
4.3. Acceptable mechanical properties
Cartilage, a smooth, flexible, and durable tissue, plays a supportive and protective role within the skeletal system. Therefore, the construction of cartilage organs requires biomaterials to provide sufficient mechanical support. As we mentioned in 3.3. Functional modification, mixing other materials can improve the mechanical strength of SF-based hydrogel. It is worth noting that the cartilage is in a constant cycle of compression and rebound. Meanwhile, during cartilage regeneration, chondrocytes are more active in a dynamic environment [158, 159]. Hence, it is preferable to construct cartilage organoids in a dynamic environment, which requires SF hydrogels with excellent anti-fatigue ability. Consider this, Huang et al. prepared host-guest interactions SF hydrogel (HG-SF hydrogel) with high remarkable anti-fatigue ability by modifying SF with cholesterol or β-cyclodextrin [160]. The hydrogel could remain in its original state after 10 times 60% stress compression without any deformation or strength decrease. Interestingly, HG-SF hydrogel could repair itself after stress injury, which showed that it had great potential to construct cartilage organoids in a dynamic environment. Additionally, our recent work found that the introduction of DNA supramolecules effectively aggregated SF molecules, inducing the formation of β-sheet structures in SF and consequently adjusting the surface rigidity of the DNA-SF hydrogels. Simultaneously, we observed that DNA-SF hydrogels with a moderate surface rigidity could induce the secretion of collagen-containing ECM by upregulating the TGF-β and Wnt signaling pathways, thereby promoting the chondrogenic differentiation of BMSCs. In vivo experimental results also demonstrated that DNA-SF hydrogels with moderate surface rigidity could expedite the cartilage repair process [137]. Based on this, Su et al. integrated photo-crosslinking with self-assembly technology to develop a novel DNA-SF hydrogel microsphere using a microfluidic system. This microsphere material offers a new option for constructing and sustaining long-term culture of cartilage organoids [161].
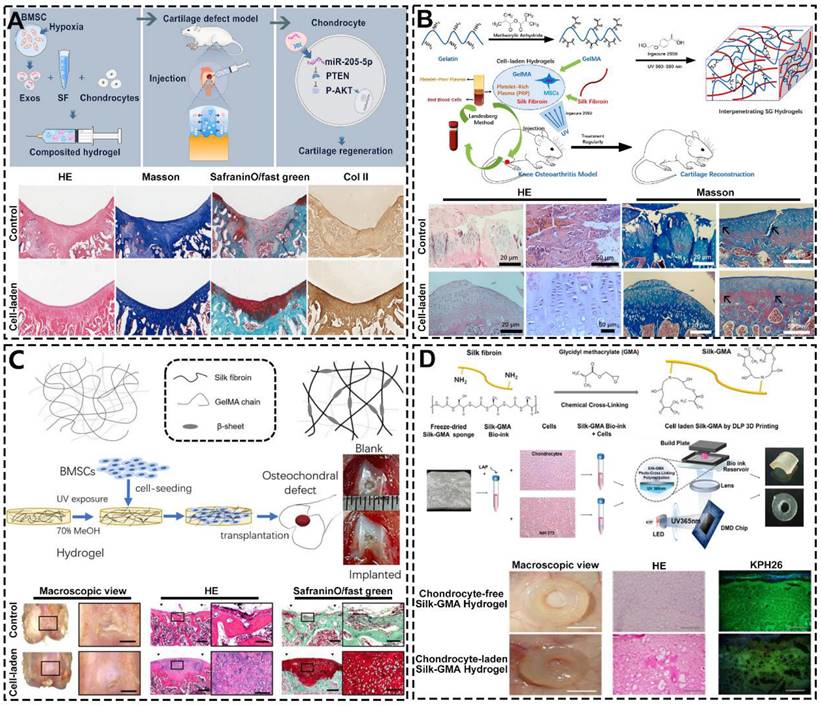
4.4. Excellent cell-laden ability
Based on its structure and chemical composition, SF-based hydrogel has excellent cell-laden ability. In the field of constructing cartilage organoids, SF-based hydrogel with excellent cell-laden ability can load chondrocytes and promote their growth and proliferation to achieve cartilage regeneration [162]. For instance, Shen et al. prepared injectable SF hydrogel containing articular chondrocytes and hypoxia preconditioned exosomes by ultrasonication (Figure 9A) [163]. They found this hydrogel significantly enhances the expression of cartilage marker genes in ACs. Additionally, histological analysis showed that the surface of the cartilage defect area repaired by cell-laden hydrogel was smooth and the regenerated cartilage arranged regularly. However, chondrocyte-laden SF hydrogels are difficult to rapidly construct cartilage organoids due to the poor mitotic activity of chondrocytes. To solve this problem, SF hydrogels can be loaded with stem cells that have the high proliferative capacity and chondrocyte differentiation potential [164, 165]. For example, Chen et al. designed and synthesized MSCs-laden GT methacrylate/SF (GelMA/SF) hydrogel with loading platelet-rich plasma (PRP) (Figure 9B) [166]. As shown by HE and Masson staining, after the intervention of MSCs-laden GelMA/SF hydrogel, the surface of articular cartilage was smooth, the chondrocytes were arranged neatly. Meanwhile, Zheng et al. constructed BMSCs-laden interpenetrating network GelMA/SF composite hydrogel through UV photo-polymerization (Figure 9C) [167]. The macroscopic results, HE and SafraninO/fast green staining showed that osteochondral repair effect of cell-laden group was significantly superior than others group. It is worth noting that the hydrogel can also match 3D biological printing technology to adapt to the regeneration and repair of a variety of cartilage tissues. For instance, Hong et al. fabricated chondrocyte-laden SF-glycidyl-methacrylate (Silk-GMA) hydrogel by using 3D bioprinting technology (Figure 9D) [168]. The in vivo experiments showed that the characteristics of the new cartilage tissue (cell morphology, proteoglycan and collagen distribution) of the chondrocyte-laden hydrogel group were closer to the natural cartilage than the chondrocyte-free hydrogel group.
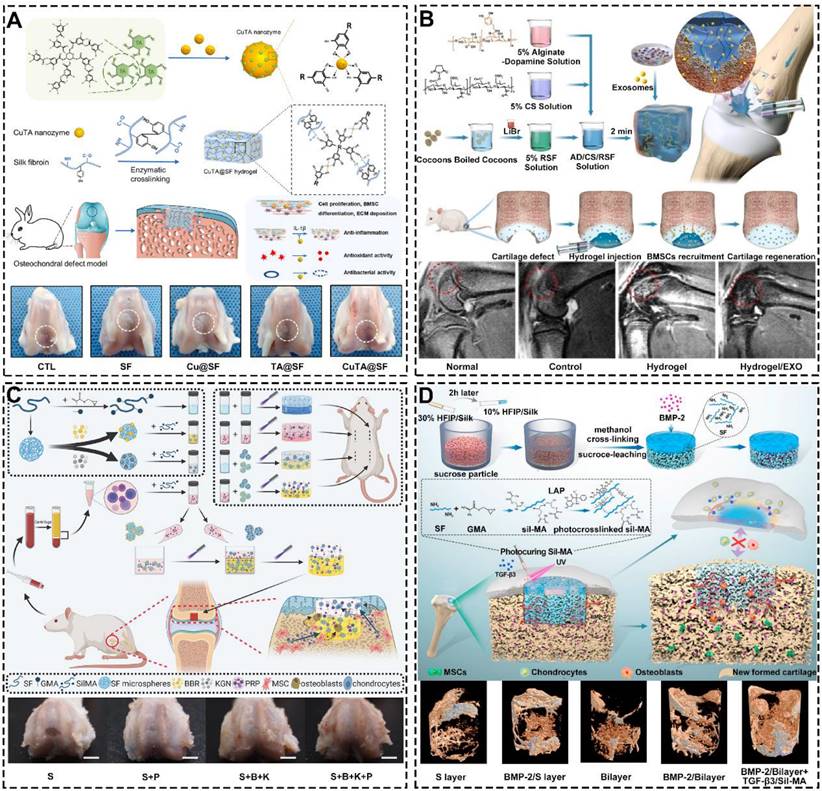
4.5. Remarkable bioactive substance delivery capacity
During natural organogenesis (from cells to organs), cells need to undergo multiple differentiations in different directions to form multiple cell populations that reassemble into functionally intact organs [169-172]. The construction of cartilage organoids parallels this process, requiring the directed induction of cells. Due to its excellent bioactive substance delivery capability, SF-based hydrogels can regulate cell proliferation, migration, and differentiation by loading polypeptides, drugs, exosomes, or growth factors [173-175]. For instance, Cao et al. developed a multifunctional silk-based hydrogel incorporated with metal-organic framework nanozymes (Figure 10A) [176]. This hydrogel had the synergistic effects of antioxidation, anti-inflammation and antibacterial, which could regulate the fate of cells and accelerate the regeneration of osteochondral defects. In addition, SF hydrogels loaded with exosomes can mimic the induction of cartilage regeneration by primary cells with no immune rejection [177-179]. For example, Zhang et al. fabricated alginate-dopamine/chondroitin sulfate/regenerated SF/exosome (AD/CS/RSF/EXO) hydrogel by enzymatic cross-linking (Figure 10B) [180]. The hydrogel had good injectability, mechanical strength and stickiness. Besides, could induce homing and chondrogenic differentiation of BMSCs. Notably, SF hydrogels loaded with growth factors regulates the migration behavior of cells. For instance, Jiang et al. prepared bilayer SilMA hydrogel loaded with Platelet-rich plasma (PRP), SF-KGN microspheres and SF-berberine (BBR) microspheres through stratified photocuring (Figure 10C) [181]. PRP enhanced the hydrogel's effect on BMSC migration and pre-differentiation, while the layered incorporation of SF-KGN and SF-BBR microspheres enabled long-term regulation of BMSC differentiation and cartilage regeneration. Meanwhile, Wu et al. constructed silk-GMA (Sil-MA) hydrogel with loading TGF-β3 through UV photo-polymerization (Figure 10D) [182]. They found that the hydrogel could promote the migration and chondrogenic differentiation of BMSCs. Importantly, the hydrogel can act as a bridge to induce integration of newborn cartilage and native cartilage. Additionally, Xia et al. utilized click chemistry to coat SF microspheres with heparin disaccharide. They then used heparin disaccharide for selective adsorption of IL-4, while LOX pDNA was preloaded onto the SF microspheres through electrostatic interactions. These functionalized SF microspheres were designed to be injected into the cartilage cavity, where they promote macrophage M2 polarization, with LOX facilitating collagen crosslinking to aid in cartilage repair [183].
5. Silk fibroin-based hydrogels in iterative optimization for cartilage organoids
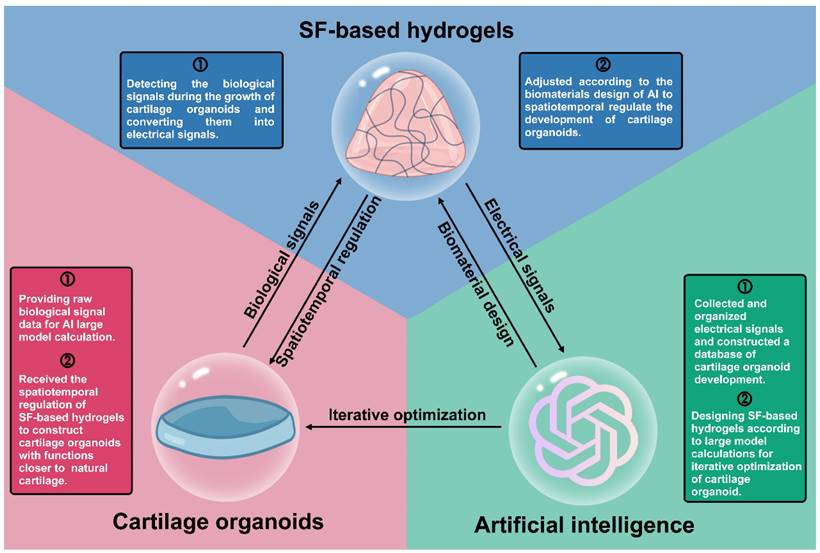
The construction of cartilage organoids is not a one-time process but requires continuous iterative optimization. To meet these needs, SF-based hydrogels must also be continuously upgraded. AI, regarded as the "design master" in life sciences, can utilize large-scale computational models to optimize the design of SF-based hydrogels, thereby enhancing their performance for cartilage organoid construction (Figure 11) [184].
Excellent cell-laden ability of SF-based hydrogels: (A) Injectable chondrocytes-laden SF-based hydrogel promoted cartilage regeneration via the miR-205-5p/PTEN/AKT pathway; Reproduced with permission from ref [163]; Copyright 2022, Elsevier. (B) MSCs-laden GelMA/SF hydrogel with the incorporation of PRP for treating osteoarthritis to reconstruct cartilage; Reproduced with permission from ref [166]; Copyright 2023, Elsevier. (C) BMSCs-laden GelMA-SF IPN hydrogel for osteochondral defect repair; Reproduced with permission from ref [167]; Copyright 2023, MDPI; (D) Digital light processing 3D printed chondrocyte-laden Silk-GMA hydrogel for trachea cartilage tissue engineering; Reproduced with permission from ref [168]; Copyright 2019, Elsevier.
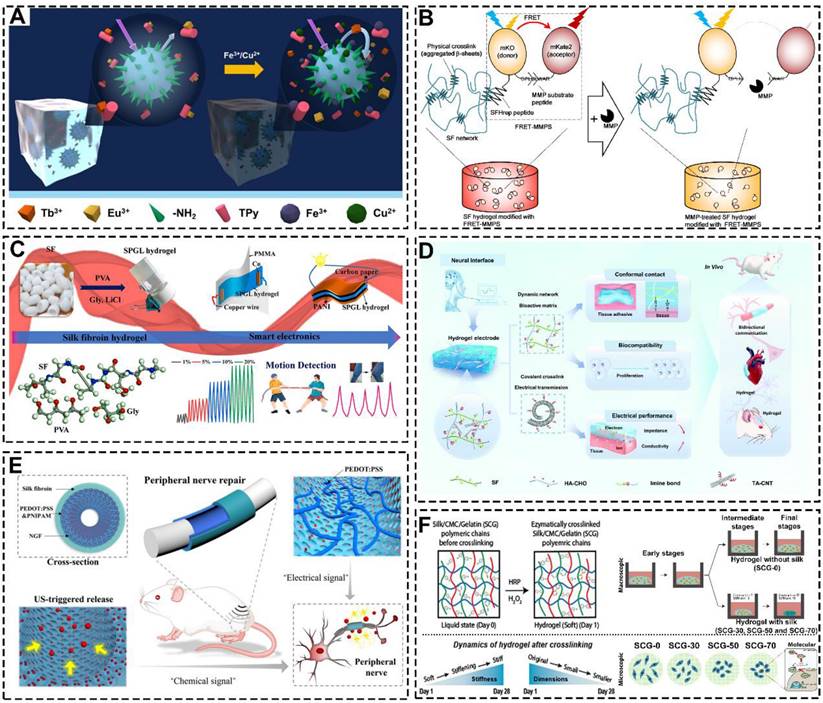
AI for large model computational design requires large amounts of data for model training [185]. SF-based hydrogels can be used as biosensors to detect biological signals during the construction of cartilage organoids. For example, Li et al. prepared a highly sensitive responsive hydrogel with SF, pectin, polyvinyl alcohol and lanthanide ions (Figure 12A) [186]. This hydrogel could specifically detect Cu2+ and Fe3+ ions. Meanwhile, Yamaoka et al. prepared a Förster/fluorescence resonance energy transfer (FRET)-based SF hydrogel (Figure 12B) [187]. This hydrogel could detect the activity of matrix metalloproteinases by FRET signal intensity. Furthermore, SF-based hydrogels can also detect physical signals generated during the construction of cartilage organoids. For example, Feng et al. Prepared mechanical detection hydrogels by combining SF with PVA/glycerol/LiCl (Figure 12C) [188]. In addition, Fan et al. constructed SF-HA-CHO hydrogel with dynamic imine crosslinking network (Figure 12D) [188]. The hydrogels were biocompatible and could detect and record intercellular electrical signals.
AI-driven iterative optimization requires hydrogels with controllable properties, and SF-based hydrogels are well-suited for functional modifications to meet these requirements. For instance, Chai et al. prepared SF-based hydrogel conduits by modifying SF with poly(3,4-ethylenedioxythiophene) and poly(4-styrene sulfonate) (Figure 12E) [189]. The hydrogel conduits achieved controlled drug release by modulating electrical signals. Additionally, Katti et al. created ternary network injectable hydrogels using SF, carboxymethyl cellulose, and GT, which showed a time-dependent contraction and stiffening effect that facilitated cartilage regeneration (Figure 12F) [190].
Remarkable bioactive substance delivery capacity of SF-based hydrogels: (A) Silk-based hydrogel incorporated with CuTA nanozymes for enhanced osteochondral defects regeneration via providing a suitable microenvironment; Reproduced with permission from ref [176]; Copyright 2022, Elsevier. (B) Injectable SF-based hydrogel with loading exosomes promoted endogenous cell recruitment and cartilage defect regeneration; Reproduced with permission from ref [180]; Copyright 2021, Elsevier. (C) SilMA bilayer hydrogel with loading BBR, KGN and PRP stimulated osteochondral defects repair; Reproduced with permission from ref [181]; Copyright 2022, Elsevier; (D) Photocurable SF-based hydrogel with loading TGF-β3 accelerated cartilage integration; Reproduced with permission from ref [182]; Copyright 2021, Elsevier.
Schematic diagram of triangular relationship between cartilage organoids, SF-based hydrogels and artificial intelligence.
6. Conclusion and Prospects
As a biomedical material with a long history of applications, SF is considered as an excellent raw material for tissue engineering hydrogels. Here, we reviewed the studies on SF hydrogels on cartilage regeneration in recent years, focusing on the preparation, functionalized modifications and advantages of SF-based hydrogels. Numerous studies demonstrated that SF hydrogels have satisfactory biological properties, suitable internal structure, acceptable mechanical properties, excellent cell-laden ability and remarkable bioactive substance delivery capacity. These features highlight the significant potential of SF hydrogels in cartilage regeneration, repair, and the construction of cartilage organoids.
Despite promising results in preclinical research, SF-based hydrogels remain largely confined to animal experimentation. Challenges persist in translating these hydrogels into clinical applications and constructing cartilage organoids due to their limited adaptability. One major obstacle lies in the inability of SF hydrogels to respond dynamically to cellular processes post-implantation, as they lack intrinsic "intelligence" or the capacity for real-time adjustment. To address these challenges, recent efforts have focused on creating intelligent SF hydrogels. For instance, Baniassadi et al. designed magnetic field responsive SF hydrogel with excellent mechanical strength and drugs delivery capability [192]. The hydrogel achieved controllable drug release by adjusting the magnetic field. In addition, researchers can attempt to combine SF-based hydrogels with programmable DNA to endow SF-based hydrogels with spatio-temporal regulatory capabilities for fine-tuning the construction of cartilage organoids [137, 193].
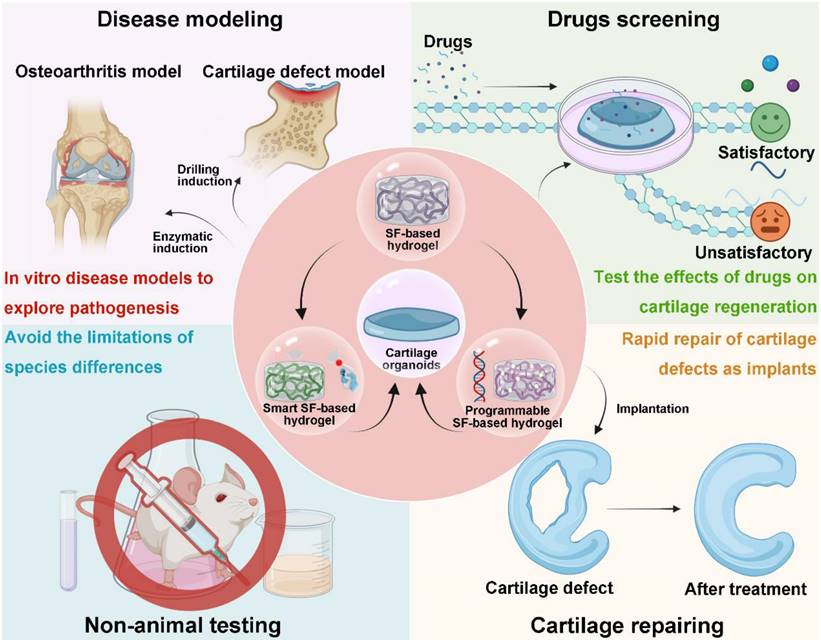
Looking forward, SF-based hydrogels offer promising avenues for advancing cartilage research and repair. Key future directions include: (1) Developing Disease Models: Cartilage organoids could be utilized to construct disease models, such as OA)or cartilage defect models, to investigate the underlying mechanisms of disease progression and tissue repair more effectively. (2) Drug Screening and Mechanistic Studies: Organoids offer a valuable platform for drug discovery, enabling researchers to screen compounds (loxoprofen sodium, KGN, D-Glucosamine sulfate, etc.) and explore their effects on cartilage regeneration. (3) Overcoming Clinical Translation Barriers: The species gap between animal models and humans remains a significant hurdle in clinical translation. Using cartilage organoids to evaluate biomaterials for regenerative functions and mechanisms can reduce reliance on animal testing and expedite clinical applications. (4) Cartilage Organoids as Implants: Due to their structural and functional similarity to native cartilage, organoids constructed from SF hydrogels could serve as implantable grafts for cartilage repair, potentially bridging the gap between tissue engineering and clinical practice (Figure 13). In conclusion, future efforts to develop smart and programmable SF hydrogels could break through the current bottlenecks in cartilage tissue engineering, offering new tools for modeling disease, discovering therapies, and advancing clinical applications. We believe that SF-based hydrogels are ideal materials for constructing cartilage organoids and can provide new approaches to cartilage regeneration research.
SF-based hydrogels detect raw biological signal data and provide precision regulation: (A) The SF-based hydrogel detects metal ions. Reproduced with permission from ref [186]; Copyright 2020, Elsevier. (B) The SF-based hydrogel detects MMP. Reproduced with permission from ref [187]; Copyright 2021, Elsevier. (C) The SF-based hydrogel detects stress stimulus. Reproduced with permission from ref [191]; Copyright 2023, Elsevier. (D) The SF-based hydrogel detects biological electrical signals. Reproduced with permission from ref [188]; Copyright 2022, Royal Society of Chemistry. (E) The SF-based hydrogel regulated cell behavior through electrical signals. Reproduced with permission from ref [189]; Copyright 2023, Wiley-VCH GmbH. (F) The SF-based hydrogels regulate chondrogenic differentiation of cells by contracting and stiffening with time contraction Reproduced with permission from ref [190]; Copyright 2022, American Chemical Society.
Development directions of SF-based hydrogels for constructing cartilage organoids: smart SF-based hydrogel and programmable SF-based hydrogel. Application prospects of cartilage organoids: disease modeling, drugs screening, non-animal testing and cartilage defects repairing. Created with BioRender.com.
Abbreviations
OA: osteoarthritis; ECM: extracellular matrix; SF: silk fibroin; AI: artificial intelligence; ACI: autologous chondrocyte implantation; MACI: mx-induced autologous chondrocyte implantation; MSCs: msenchymal stem cells; COs: callus organoids; HRP: horseradish peroxidase; TA: tyramine; GT: gelatin; SF C-gel: SF hydrogels by using Co-60 derived gamma-ray; GTA: glutaraldehyde; SF/PCZ: polycarbazole/silk fibroin hydrogels; KGN: kartogenin; PDGF-BB: platelet-derived growth factor BB; BSNF: beta-sheet rich silk nanofibers; BMSCs: bone marrow mesenchymal stem cells; RSF: regenerated silk fibroin; PEG: polyethylene glycol; PEGDMA: poly(ethylene glycol) dimethacrylate; SilMA: silk methacrylate; DN: double network; ALG-POL: alginate-poloxamer; Col: collagen; HA: hyaluronic acid; GA: glycyrrhizic acid; IPN: interpenetrating network; HPMC: hydroxypropyl methyl cellulose; CS: chitosan; PC: propanoic acid-modified chitosan; DNA: deoxyribonucleic acid; HG-SF: host-guest interactions silk fibroin; GelMA: gelatin methacrylate; Silk-GMA: SF-glycidyl-methacrylate; AD/CS/RSF/EXO: alginate-dopamine/chondroitin sulfate/regenerated silk fibroin/exosome hydrogel; BBR: berberine; FRET: förster/fluorescence resonance energy transfer.
Acknowledgements
This work was supported by the National Key Research and Development Program of China (No. 2022YFB3804300), Integrated Project of Major Research Plan of National Natural Science Foundation of China (92249303), Key Project of the National Natural Science Foundation of China (82230071), National Natural Science Foundation of China (82172098 and 32471395), Shanghai Science and Technology Innovation Action Plan (23141900600), Research Physician Training Program of Shanghai Hospital Development Center (SHDC2023CRT013), and Shanghai Municipal Demonstration Project for Innovative Medical Device Applications (23SHS05700).
Author contributions
Congyi Shen, Ziyang Zhou, Ruiyang Li and Shike Yang contributed equally to this work. Congyi Shen: Conceptualization, Writing - original draft, Writing - review & editing. Ziyang Zhou: Writing - original draft, Writing - review & editing. Ruiyang Li: Writing - review & editing. Shike Yang: Writing - review & editing. Dongyang Zhou: Writing - review & editing. Fengjin Zhou: Writing - review & editing, Supervision. Zhen Geng: Writing - review & editing, Funding acquisition. Jiacan Su: Funding acquisition, Supervision. All authors read and approved the final manuscript.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Collins KH, Lenz KL, Pollitt EN, Ferguson D, Hutson I, Springer LE. et al. Adipose tissue is a critical regulator of osteoarthritis. Proc Natl Acad Sci U S A. 2021;118:e2021096118
2. Xue X, Liu H, Wang S, Hu Y, Huang B, Li M. et al. Neutrophil-erythrocyte hybrid membrane-coated hollow copper sulfide nanoparticles for targeted and photothermal/anti-inflammatory therapy of osteoarthritis. Compos B Eng. 2022;237:109855
3. Peng Z, Sun H, Bunpetch V, Koh Y, Wen Y, Wu D. et al. The regulation of cartilage extracellular matrix homeostasis in joint cartilage degeneration and regeneration. Biomaterials. 2021;268:120555
4. Zheng L, Zhang Z, Sheng P, Mobasheri A. The role of metabolism in chondrocyte dysfunction and the progression of osteoarthritis. Ageing Res Rev. 2021;66:101249
5. Hu Y, Chen X, Wang S, Jing Y, Su J. Subchondral bone microenvironment in osteoarthritis and pain. Bone Res. 2021;9:20
6. Safiri S, Kolahi AA, Smith E, Hill C, Bettampadi D, Mansournia MA. et al. Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the Global Burden of Disease Study 2017. Ann Rheum Dis. 2020;79:819-28
7. Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393:1745-59
8. Gao J, Pei H, Lv F, Niu X, You Y, He L. et al. JD-312 - A novel small molecule that facilitates cartilage repair and alleviates osteoarthritis progression. J Orthop Translat. 2024;44:60-71
9. Steinmetz JD, Culbreth GT, Haile LM, Rafferty Q, Lo J, Fukutaki KG. et al. Global, regional, and national burden of osteoarthritis, 1990-2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5:e508-e22
10. van den Bosch MHJ. Osteoarthritis year in review 2020: biology. Osteoarthritis Cartilage. 2021;29:143-50
11. Liang M, Wang K, Wei X, Gong X, Tang H, Xue H. et al. Replenishing decoy extracellular vesicles inhibits phenotype remodeling of tissue-resident cells in inflammation-driven arthritis. Cell Rep Med. 2023;4:101228
12. Onnerfjord P, Khabut A, Reinholt FP, Svensson O, Heinegard D. Quantitative proteomic analysis of eight cartilaginous tissues reveals characteristic differences as well as similarities between subgroups. J Biol Chem. 2012;287:18913-24
13. Vilela CA, Correia C, Oliveira JM, Sousa RA, Espregueira-Mendes J, Reis RL. Cartilage Repair Using Hydrogels: A Critical Review of in Vivo Experimental Designs. ACS Biomater Sci Eng. 2015;1:726-39
14. Zhang W, Ouyang H, Dass CR, Xu J. Current research on pharmacologic and regenerative therapies for osteoarthritis. Bone Res. 2016;4:15040
15. Hofer M, Lutolf MP. Engineering organoids. Nat Rev Mater. 2021;6:402-20
16. Drakhlis L, Biswanath S, Farr CM, Lupanow V, Teske J, Ritzenhoff K. et al. Human heart-forming organoids recapitulate early heart and foregut development. Nat Biotechnol. 2021;39:737-46
17. Ma Z, Wu Y, Li G, Liu J, Geng Z, Su J. Extracellular vesicles-loaded DNA hydrogels: A promising candidate for cartilage organoids engineering. Chem Eng J. 2023;477:147146
18. Shen C, Li Z, Li G, Wang G, Geng Z, Su J. DNA-based hydrogels: Ideal biomaterials for cartilage organoids. Fundam Res. 2024
19. Crispim JF, Ito K. De novo neo-hyaline-cartilage from bovine organoids in viscoelastic hydrogels. Acta Biomater. 2021;128:236-49
20. Singh YP, Moses JC, Bhardwaj N, Mandal BB. Injectable hydrogels: a new paradigm for osteochondral tissue engineering. J Mater Chem B. 2018;6:5499-529
21. Galperin A, Oldinski RA, Florczyk SJ, Bryers JD, Zhang M, Ratner BD. Integrated bi-layered scaffold for osteochondral tissue engineering. Adv Healthc Mater. 2013;2:872-83
22. Zhao X, Hu DA, Wu D, He F, Wang H, Huang L. et al. Applications of Biocompatible Scaffold Materials in Stem Cell-Based Cartilage Tissue Engineering. Front Bioeng Biotechnol. 2021;9:603444
23. Chen S, Chen X, Geng Z, Su J. The horizon of bone organoid: A perspective on construction and application. Bioact Mater. 2022;18:15-25
24. Gai T, Zhang Y, Li G, Zhou F, He C, Wang X. et al. Engineered hydrogel microspheres for spheroids and organoids construction. Chem Eng J. 2024;498:155131
25. Kaur S, Kaur I, Rawal P, Tripathi DM, Vasudevan A. Non-matrigel scaffolds for organoid cultures. Cancer Lett. 2021;504:58-66
26. Holland C, Numata K, Rnjak-Kovacina J, Seib FP. The Biomedical Use of Silk: Past, Present, Future. Adv Healthc Mater. 2019;8:e1800465
27. Johari N, Khodaei A, Samadikuchaksaraei A, Reis RL, Kundu SC, Moroni L. Ancient fibrous biomaterials from silkworm protein fibroin and spider silk blends: Biomechanical patterns. Acta Biomater. 2022;153:38-67
28. Ju Y-X, Hu R-Z, Wang P-Y, Shen Y-S, Shuang F-F, Wang J. et al. Strong Silk Fibroin/PVA/Chitosan Hydrogels with High Water Content Inspired by Straw Rammed Earth Brick Structures. ACS Sustain Chem Eng. 2022;10:13070-80
29. Shuang F-F, Zong C-M, Wang C-C, Hu R-Z, Shen Y-S, Ju Y-X. et al. Chlorogenic acid and cellulose nanocrystal-assisted crosslinking preparation of a silk-based film to extend the shelf life of strawberries. LWT-Food Sci. Technol. 2022;172:114218
30. Laomeephol C, Ferreira H, Kanokpanont S, Luckanagul JA, Neves NM, Damrongsakkul S. Osteogenic differentiation of encapsulated cells in dexamethasone-loaded phospholipid-induced silk fibroin hydrogels. Biomater Transl. 2022;3:213-20
31. Ribeiro VP, Pina S, Oliveira JM, Reis RL. Silk Fibroin-Based Hydrogels and Scaffolds for Osteochondral Repair and Regeneration. Adv Exp Med Biol. 2018;1058:305-25
32. Qiu W, Liu XY. Recent Progress of Applying Mesoscopic Functionalization Engineering Principles to Spin Advanced Regenerated Silk Fibroin Fibers. Adv Fiber Mater. 2022;4:390-403
33. Liu H, Sun Z, Guo C. Chemical Modification of Silk Proteins: Current Status and Future Prospects. Adv Fiber Mater. 2022;4:705-19
34. Costa JB, Silva-Correia J, Ribeiro VP, Morais AD, Oliveira JM, Reis RL. Engineering patient-specific bioprinted constructs for treatment of degenerated intervertebral disc. Mater Today Commun. 2019;19:506-12
35. Bhar B, Das E, Manikumar K, Mandal BB. 3D Bioprinted Human Skin Model Recapitulating Native-Like Tissue Maturation and Immunocompetence as an Advanced Platform for Skin Sensitization Assessment. Adv Healthc Mater. 2024;13:2303312
36. Li XL, Sheng SH, Li GF, Hu Y, Zhou FJ, Geng Z. et al. Research Progress in Hydrogels for Cartilage Organoids. Adv Healthc Mater. 2024;13:2400431
37. Wang HY, Zhang YQ. Processing silk hydrogel and its applications in biomedical materials. Biotechnol Prog. 2015;31:630-40
38. Myatt JP, Schilling N, Thorpe SK. Distribution patterns of fibre types in the triceps surae muscle group of chimpanzees and orangutans. J Anat. 2011;218:402-12
39. Taheri S, Ghazali HS, Ghazali ZS, Bhattacharyya A, Noh I. Correction: Progress in biomechanical stimuli on the cell-encapsulated hydrogels for cartilage tissue regeneration. Biomater Res. 2023;27:74
40. Taheri S, Ghazali HS, Ghazali ZS, Bhattacharyya A, Noh I. Progress in biomechanical stimuli on the cell-encapsulated hydrogels for cartilage tissue regeneration. Biomater Res. 2023;27:22
41. Li MM, Yu B, Wang SC, Zhou FJ, Cui J, Su JC. Microenvironment-responsive nanocarriers for targeted bone disease therapy. Nano Today. 2023;50:101838
42. Wei W, Dai H. Articular cartilage and osteochondral tissue engineering techniques: Recent advances and challenges. Bioact Mater. 2021;6:4830-55
43. Zimmermann. B, Wachtel. HC, Somogyi. H. Endochondral mineralization in cartilage organoid culture. Cell Differ Dev. 1990;31:11-22
44. Albro MB, Nims RJ, Durney KM, Cigan AD, Shim JJ, Vunjak-Novakovic G. et al. Heterogeneous engineered cartilage growth results from gradients of media-supplemented active TGF-beta and is ameliorated by the alternative supplementation of latent TGF-beta. Biomaterials. 2016;77:173-85
45. Takada E, Mizuno S. Reproduction of Characteristics of Extracellular Matrices in Specific Longitudinal Depth Zone Cartilage within Spherical Organoids in Response to Changes in Osmotic Pressure. Int J Mol Sci. 2018;19:1507
46. Rothbauer M, Byrne RA, Schobesberger S, Olmos Calvo I, Fischer A, Reihs EI. et al. Establishment of a human three-dimensional chip-based chondro-synovial coculture joint model for reciprocal cross talk studies in arthritis research. Lab Chip. 2021;21:4128-43
47. Wei J, Baptista-Hon DT, Wang Z, Li G, Herrler T, Dai C. et al. Bioengineered human tissue regeneration and repair using endogenous stem cells. Cell Rep Med. 2023;4:101156
48. Cao. Y, Vacanti. JP, Paige. KT, Upton. J, Vacanti. CA. Transplantation of Chondrocytes Utilizing a Polymer-Cell Construct to Produce Tissue-Engineered Cartilage in the Shape of a Human Ear. Plast. Reconstr. Surg. 1997;100:297-302
49. Zhang L, He A, Yin Z, Yu Z, Luo X, Liu W. et al. Regeneration of human-ear-shaped cartilage by co-culturing human microtia chondrocytes with BMSCs. Biomaterials. 2014;35:4878-87
50. Jeon O, Lee YB, Jeong H, Lee SJ, Wells D, Alsberg E. Individual cell-only bioink and photocurable supporting medium for 3D printing and generation of engineered tissues with complex geometries. Mater Horiz. 2019;6:1625-31
51. Wang Q, Ran X, Wang J, Wang S, Zhang P, Gao E. et al. Elastic Fiber-Reinforced Silk Fibroin Scaffold with A Double-Crosslinking Network for Human Ear-Shaped Cartilage Regeneration. Adv Fiber Mater. 2023;5:1008-1024
52. Xing D, Liu W, Li JJ, Liu L, Guo A, Wang B. et al. Engineering 3D functional tissue constructs using self-assembling cell-laden microniches. Acta Biomater. 2020;114:170-82
53. Xiahou Z, She Y, Zhang J, Qin Y, Li G, Zhang L. et al. Designer Hydrogel with Intelligently Switchable Stem-Cell Contact for Incubating Cartilaginous Microtissues. ACS Appl Mater Interfaces. 2020;12:40163-75
54. Hall GN, Tam WL, Andrikopoulos KS, Casas-Fraile L, Voyiatzis GA, Geris L. et al. Patterned, organoid-based cartilaginous implants exhibit zone specific functionality forming osteochondral-like tissues in vivo. Biomaterials. 2021;273:120820
55. Abe K, Yamashita A, Morioka M, Horike N, Takei Y, Koyamatsu S. et al. Engraftment of allogeneic iPS cell-derived cartilage organoid in a primate model of articular cartilage defect. Nat Commun. 2023;14:804
56. Yang Z, Wang B, Liu W, Li X, Liang K, Fan Z. et al. In situ self-assembled organoid for osteochondral tissue regeneration with dual functional units. Bioact Mater. 2023;27:200-15
57. Wen Y, Chen Y, Wu W, Zhang H, Peng Z, Yao X. et al. Hyperplastic Human Macromass Cartilage for Joint Regeneration. Adv Sci (Weinh). 2023;10:2301833
58. Farokhi M, Aleemardani M, Solouk A, Mirzadeh H, Teuschl AH, Redl H. Crosslinking strategies for silk fibroin hydrogels: promising biomedical materials. Biomed Mater. 2021;16:022004
59. Zhou Z, Cui J, Wu S, Geng Z, Su J. Silk fibroin-based biomaterials for cartilage/osteochondral repair. Theranostics. 2022;12:5103-24
60. Schneider KH, Goldberg BJ, Hasturk O, Mu X, Dotzlhofer M, Eder G. et al. Silk fibroin, gelatin, and human placenta extracellular matrix-based composite hydrogels for 3D bioprinting and soft tissue engineering. Biomater Res. 2023;27:117
61. Kapoor S, Kundu SC. Silk protein-based hydrogels: Promising advanced materials for biomedical applications. Acta Biomater. 2016;31:17-32
62. Liu J, Ge X, Liu L, Xu W, Shao R. Challenges and opportunities of silk protein hydrogels in biomedical applications. Mater Adv. 2022;3:2291-308
63. Wang ZX, Yin XY, Zhuang CY, Wu K, Wang HR, Shao ZZ. et al. Injectable Regenerated Silk Fibroin Micro/Nanosphere with Enhanced Permeability and Stability for Osteoarthritis Therapy. Small. 2024;20:e2405049
64. Floren M, Migliaresi C, Motta A. Processing Techniques and Applications of Silk Hydrogels in Bioengineering. J Funct Biomater. 2016;7:7030026
65. Sun W, Gregory DA, Tomeh MA, Zhao X. Silk Fibroin as a Functional Biomaterial for Tissue Engineering. Int J Mol Sci. 2021;22:1499
66. Lin KL, Zhang DW, Macedo MH, Cui WG, Sarmento B, Shen GF. Advanced Collagen-Based Biomaterials for Regenerative Biomedicine. Adv Funct Mater. 2019;29:1804943
67. Dong LP, Liu QL, Gao YL, Jia HX, Dai WL, Guo LK. et al. The effect of collagen hydrogels on chondrocyte behaviors through restricting the contraction of cell/hydrogel constructs. Regen Biomater. 2021;8:rbab030
68. Sahoo DR, Biswal T. Alginate and its application to tissue engineering. SN Appl Sci. 2021;3:30
69. Venkatesan J, Bhatnagar I, Manivasagan P, Kang KH, Kim SK. Alginate composites for bone tissue engineering: A review. Int J Biol Macromol. 2015;72:269-81
70. Smith AM, Senior JJ. Alginate Hydrogels with Tuneable Properties. Adv Biochem Eng Biotechnol. 2021;178:37-61
71. Hu YP, Liu NN, Chen K, Liu MX, Wang F, Liu P. et al. Resilient and Self-Healing Hyaluronic Acid/Chitosan Hydrogel With Ion Conductivity, Low Water Loss, and Freeze-Tolerance for Flexible and Wearable Strain Sensor. Front Bioeng Biotechnol. 2022;10:837750
72. Tavsanli B, Okay O. Mechanically strong hyaluronic acid hydrogels with an interpenetrating network structure. Eur Polym J. 2017;94:185-95
73. Borries M, Barooji YF, Yennek S, Grapin-Botton A, Berg-Sorensen K, Oddershede LB. Quantification of Visco-Elastic Properties of a Matrigel for Organoid Development as a Function of Polymer Concentration. Front Phys. 2020;8:579168
74. Méhes E, Biri-Kovács B, Isai DG, Gulyás M, Nyitray L, Czirók A. Matrigel patterning reflects multicellular contractility. PLoS Comput Biol. 2019;15:e1007431
75. Passaniti A, Kleinman HK, Martin GR. Matrigel: history/background, uses, and future applications. J Cell Commun Signal. 2022;16:621-6
76. Wongpinyochit T, Johnston BF, Seib FP. Degradation Behavior of Silk Nanoparticles-Enzyme Responsiveness. ACS Biomater Sci Eng. 2018;4:942-51
77. Shuang F F, Wang C C, Zhu W J, Chen T, Yao X H, Zhang D Y. et al. Preparation of a robust silk fibroin scaffold with a reinforced concrete structure constructed with silk nanofibers as the skeleton based on a CaCl2-formic acid solution and freeze-drying method. Polym Test. 2022;111:107599
78. Yang C, Li S, Huang X, Chen X, Shan H, Chen X. et al. Silk Fibroin Hydrogels Could Be Therapeutic Biomaterials for Neurological Diseases. Oxid Med Cell Longev. 2022;2022:2076680
79. Teixeira LS, Feijen J, van Blitterswijk CA, Dijkstra PJ, Karperien M. Enzyme-catalyzed crosslinkable hydrogels: emerging strategies for tissue engineering. Biomaterials. 2012;33:1281-90
80. Chen F, Yu S, Liu B, Ni Y, Yu C, Su Y. et al. An Injectable Enzymatically Crosslinked Carboxymethylated Pullulan/Chondroitin Sulfate Hydrogel for Cartilage Tissue Engineering. Sci Rep. 2016;6:20014
81. Chen W, Fu M, Zhu X, Liu Q. Protein recognition by polydopamine-based molecularly imprinted hollow spheres. Biosens Bioelectron. 2019;142:111492
82. Chen W, Fu M, Zhu X, Liu Q. A close-packed imprinted colloidal array for naked-eye detection of glycoproteins under physiological pH. Biosens Bioelectron. 2019;142:111499
83. Tabatabai AP, Partlow BP, Raia NR, Kaplan DL, Blair DL. Silk Molecular Weight Influences the Kinetics of Enzymatically Cross-linked Silk Hydrogel Formation. Langmuir. 2018;34:15383-7
84. Chen W, Zhang L, Sun Y, Yu H, Fu M. pH-Responsive molecularly imprinted hollow spheres for selective separation of ribavirin from water samples. Chem Eng J. 2022;450:138064
85. Partlow BP, Hanna CW, Rnjak-Kovacina J, Moreau JE, Applegate MB, Burke KA. et al. Highly tunable elastomeric silk biomaterials. Adv Funct Mater. 2014;24:4615-24
86. Hasturk O, Jordan KE, Choi J, Kaplan DL. Enzymatically crosslinked silk and silk-gelatin hydrogels with tunable gelation kinetics, mechanical properties and bioactivity for cell culture and encapsulation. Biomaterials. 2020;232:119720
87. Li Q, Xu S, Feng Q, Dai Q, Yao L, Zhang Y. et al. 3D printed silk-gelatin hydrogel scaffold with different porous structure and cell seeding strategy for cartilage regeneration. Bioact Mater. 2021;6:3396-410
88. Wang L, Zhang YF, Xia YJ, Xu CZ, Meng KJ, Lian J. et al. Photocross-linked silk fibroin/hyaluronic acid hydrogel loaded with hDPSC for pulp regeneration. Int J Biol Macromol. 2022;215:155-68
89. Annabi N, Tamayol A, Uquillas JA, Akbari M, Bertassoni LE, Cha C. et al. 25th anniversary article: Rational design and applications of hydrogels in regenerative medicine. Adv Mater. 2014;26:85-123
90. Piluso S, Flores Gomez D, Dokter I, Moreira Texeira L, Li Y, Leijten J. et al. Rapid and cytocompatible cell-laden silk hydrogel formation via riboflavin-mediated crosslinking. J Mater Chem B. 2020;8:9566-75
91. Cui X, Soliman BG, Alcala-Orozco CR, Li J, Vis MAM, Santos M. et al. Rapid Photocrosslinking of Silk Hydrogels with High Cell Density and Enhanced Shape Fidelity. Adv Healthc Mater. 2020;9:e1901667
92. Kim MH, Kim BS, Lee J, Cho D, Kwon OH, Park WH. Silk fibroin/hydroxyapatite composite hydrogel induced by gamma-ray irradiation for bone tissue engineering. Biomater Res. 2017;21:12
93. Kim MH, Park WH. Chemically cross-linked silk fibroin hydrogel with enhanced elastic properties, biodegradability, and biocompatibility. Int J Nanomedicine. 2016;11:2967-78
94. Zheng H, Zuo B. Functional silk fibroin hydrogels: preparation, properties and applications. J Mater Chem B. 2021;9:1238-58
95. Srisawasdi T, Petcharoen K, Sirivat A, Jamieson AM. Electromechanical response of silk fibroin hydrogel and conductive polycarbazole/silk fibroin hydrogel composites as actuator material. Mater Sci Eng C Mater Biol Appl. 2015;56:1-8
96. Min Q, Tian D, Zhang Y, Wang C, Wan Y, Wu J. Strong and Elastic Chitosan/Silk Fibroin Hydrogels Incorporated with Growth-Factor-Loaded Microspheres for Cartilage Tissue Engineering. Biomimetics (Basel). 2022;7:41
97. Wang W, Nema S, Teagarden D. Protein aggregation-pathways and influencing factors. Int J Pharm. 2010;390:89-99
98. Nagarkar S, Nicolai T, Chassenieux C, Lele A. Structure and gelation mechanism of silk hydrogels. Phys Chem Chem Phys. 2010;12:3834-44
99. Kim U-J, Park J, Li C, Jin H-J, Valluzzi R, Kaplan DL. Structure and properties of silk hydrogels. Biomacromolecules. 2004;5:786-92
100. Nagarkar S, Patil A, Lele A, Bhat S, Bellare J, Mashelkar RA. Some Mechanistic Insights into the Gelation of Regenerated Silk Fibroin Sol. Ind Eng Chem Res. 2009;48:8014-23
101. Fini M, Motta A, Torricelli P, Giavaresi G, Nicoli Aldini N, Tschon M. et al. The healing of confined critical size cancellous defects in the presence of silk fibroin hydrogel. Biomaterials. 2005;26:3527-36
102. Kojic N, Pritchard EM, Tao H, Brenckle MA, Mondia JP, Panilaitis B. et al. Focal Infection Treatment using Laser-Mediated Heating of Injectable Silk Hydrogels with Gold Nanoparticles. Adv Funct Mater. 2012;22:3793-8
103. Davis NE, Beenken-Rothkopf LN, Mirsoian A, Kojic N, Kaplan DL, Barron AE. et al. Enhanced function of pancreatic islets co-encapsulated with ECM proteins and mesenchymal stromal cells in a silk hydrogel. Biomaterials. 2012;33:6691-7
104. Chen D, Yin Z, Wu F, Fu H, Kundu SC, Lu S. Orientational behaviors of silk fibroin hydrogels. J Appl Polym Sci. 2017;134:45050
105. Kasoju N, Hawkins N, Pop-Georgievski O, Kubies D, Vollrath F. Silk fibroin gelation via non-solvent induced phase separation. Biomater Sci. 2016;4:460-73
106. Wang X, Kluge JA, Leisk GG, Kaplan DL. Sonication-induced gelation of silk fibroin for cell encapsulation. Biomaterials. 2008;29:1054-64
107. Yuan T, Li Z, Zhang Y, Shen K, Zhang X, Xie R. et al. Injectable Ultrasonication-Induced Silk Fibroin Hydrogel for Cartilage Repair and Regeneration. Tissue Eng Part A. 2021;27:1213-24
108. Byram PK, Sunka KC, Barik A, Kaushal M, Dhara S, Chakravorty N. Biomimetic silk fibroin and xanthan gum blended hydrogels for connective tissue regeneration. Int J Biol Macromol. 2020;165:874-82
109. Leisk GG, Lo TJ, Yucel T, Lu Q, Kaplan DL. Electrogelation for protein adhesives. Adv Mater. 2010;22:711-5
110. Liu H, Ming J, Guo X, Huang X, Zuo B, Ning X. Low voltage electric field governs fibrous silk electrogels. Mater Des. 2021;199:109401
111. Xu G, Ding Z, Lu Q, Zhang X, Zhou X, Xiao L. et al. Electric field-driven building blocks for introducing multiple gradients to hydrogels. Protein Cell. 2020;11:267-85
112. Wang B, Yuan S, Xin W, Chen Y, Fu Q, Li L. et al. Synergic adhesive chemistry-based fabrication of BMP-2 immobilized silk fibroin hydrogel functionalized with hybrid nanomaterial to augment osteogenic differentiation of rBMSCs for bone defect repair. Int J Biol Macromol. 2021;192:407-16
113. Balu R, Reeder S, Knott R, Mata J, de Campo L, Dutta NK. et al. Tough Photocrosslinked Silk Fibroin/Graphene Oxide Nanocomposite Hydrogels. Langmuir. 2018;34:9238-51
114. Zhang Y, Cao Y, Zhang L, Zhao H, Ni T, Liu Y. et al. Fabrication of an injectable BMSC-laden double network hydrogel based on silk fibroin/PEG for cartilage repair. J Mater Chem B. 2020;8:5845-8
115. Fathi-Achachelouei M, Keskin D, Bat E, Vrana NE, Tezcaner A. Dual growth factor delivery using PLGA nanoparticles in silk fibroin/PEGDMA hydrogels for articular cartilage tissue engineering. J Biomed Mater Res B Appl Biomater. 2020;108:2041-62
116. Bandyopadhyay A, Mandal BB, Bhardwaj N. 3D bioprinting of photo-crosslinkable silk methacrylate (SilMA)-polyethylene glycol diacrylate (PEGDA) bioink for cartilage tissue engineering. J Biomed Mater Res A. 2022;110:884-98
117. Whittaker JL, Dutta NK, Zannettino A, Choudhury NR. Engineering DN hydrogels from regenerated silk fibroin and poly(N-vinylcaprolactam). J Mater Chem B. 2016;4:5519-33
118. Allur Subramanian S, Oh S, Mariadoss AVA, Chae S, Dhandapani S, Parasuraman PS. et al. Tunable mechanical properties of Mo3Se3-poly vinyl alcohol-based/silk fibroin-based nanowire ensure the regeneration mechanism in tenocytes derived from human bone marrow stem cells. Int J Biol Macromol. 2022;210:196-207
119. Min Q, Liu J, Zhang Y, Yang B, Wan Y, Wu J. Dual Network Hydrogels Incorporated with Bone Morphogenic Protein-7-Loaded Hyaluronic Acid Complex Nanoparticles for Inducing Chondrogenic Differentiation of Synovium-Derived Mesenchymal Stem Cells. Pharmaceutics. 2020;12:613
120. Liu J, Fang Q, Lin H, Yu X, Zheng H, Wan Y. Alginate-poloxamer/silk fibroin hydrogels with covalently and physically cross-linked networks for cartilage tissue engineering. Carbohydr Polym. 2020;247:116593
121. Hu ZC, Lu JQ, Zhang TW, Liang HF, Yuan H, Su DH. et al. Piezoresistive MXene/Silk fibroin nanocomposite hydrogel for accelerating bone regeneration by Re-establishing electrical microenvironment. Bioact Mater. 2023;22:1-17
122. Yang ZZ, You YX, Liu XY, Wan Q, Xu ZP, Shuai YJ. et al. Injectable Bombyx mori (B. mori) silk fibroin/MXene conductive hydrogel for electrically stimulating neural stem cells into neurons for treating brain damage. J Nanobiotechnology. 2024;22:111
123. Long S, Huang D, Ma Z, Shi S, Xiao Y, Zhang X. A sonication-induced silk-collagen hydrogel for functional cartilage regeneration. J Mater Chem B. 2022;10:5045-57
124. Zhang Y, Liu M, Pei R. An in situ gelling BMSC-laden collagen/silk fibroin double network hydrogel for cartilage regeneration. Mater Adv. 2021;2:4733-42
125. Trucco D, Sharma A, Manferdini C, Gabusi E, Petretta M, Desando G. et al. Modeling and Fabrication of Silk Fibroin-Gelatin-Based Constructs Using Extrusion-Based Three-Dimensional Bioprinting. ACS Biomater Sci Eng. 2021;7:3306-20
126. Park S, Edwards S, Hou S, Boudreau R, Yee R, Jeong KJ. A multi-interpenetrating network (IPN) hydrogel with gelatin and silk fibroin. Biomater Sci. 2019;7:1276-80
127. Luo K, Yang Y, Shao Z. Physically Crosslinked Biocompatible Silk-Fibroin-Based Hydrogels with High Mechanical Performance. Adv Funct Mater. 2016;26:872-80
128. Mirahmadi F, Tafazzoli-Shadpour M, Shokrgozar MA, Bonakdar S. Enhanced mechanical properties of thermosensitive chitosan hydrogel by silk fibers for cartilage tissue engineering. Mater Sci Eng C Mater Biol Appl. 2013;33:4786-94
129. Xu Z, Tang E, Zhao H. An Environmentally Sensitive Silk Fibroin/Chitosan Hydrogel and Its Drug Release Behaviors. Polymers (Basel). 2019;11:1980
130. Yu Y, Yu X, Tian D, Yu A, Wan Y. Thermo-responsive chitosan/silk fibroin/amino-functionalized mesoporous silica hydrogels with strong and elastic characteristics for bone tissue engineering. Int J Biol Macromol. 2021;182:1746-58
131. Dong Y, Liu Y, Chen Y, Sun X, Zhang L, Zhang Z. et al. Spatiotemporal regulation of endogenous MSCs using a functional injectable hydrogel system for cartilage regeneration. NPG Asia Mater. 2021;13:71
132. Weitkamp JT, Woltje M, Nusspickel B, Schmidt FN, Aibibu D, Bayer A. et al. Silk Fiber-Reinforced Hyaluronic Acid-Based Hydrogel for Cartilage Tissue Engineering. Int J Mol Sci. 2021;22:3635
133. Ziadlou R, Rotman S, Teuschl A, Salzer E, Barbero A, Martin I. et al. Optimization of hyaluronic acid-tyramine/silk-fibroin composite hydrogels for cartilage tissue engineering and delivery of anti-inflammatory and anabolic drugs. Mater Sci Eng C Mater Biol Appl. 2021;120:111701
134. Wang X, Song X, Li T, Chen J, Cheng G, Yang L. et al. Aptamer-Functionalized Bioscaffold Enhances Cartilage Repair by Improving Stem Cell Recruitment in Osteochondral Defects of Rabbit Knees. Am J Sports Med. 2019;47:2316-26
135. Ding J, Chen ZH, Liu XY, Tian Y, Jiang J, Qiao Z. et al. A mechanically adaptive hydrogel neural interface based on silk fibroin for high-efficiency neural activity recording. Mater Horiz. 2022;9:2215-25
136. Zhang BC, Wang WS, Gao P, Li X, Chen LL, Lin ZF. et al. Injectable, Electroconductive, Free Radical Scavenging Silk Fibroin/Black Phosphorus/Glycyrrhizic Acid Nanocomposite Hydrogel for Enhancing Spinal Cord Repair. Adv Healthc Mater. 2024;13:2304300
137. Zhou Z, Song P, Wu Y, Wang M, Shen C, Ma Z. et al. Dual-network DNA-Silk fibroin hydrogels with controllable surface rigidity for regulating chondrogenic differentiation. Mater Horiz. 2024;11:1465-1483
138. Zhao Y, Zhu ZS, Guan J, Wu SJ. Processing, mechanical properties and bio-applications of silk fibroin-based high-strength hydrogels. Acta Biomater. 2021;125:57-71
139. Kim JS, Choi J, Ki CS, Lee KH. 3D Silk Fiber Construct Embedded Dual-Layer PEG Hydrogel for Articular Cartilage Repair - In vitro Assessment. Front Bioeng Biotechnol. 2021;9:653509
140. Kim SH, Hong H, Ajiteru O, Sultan MT, Lee YJ, Lee JS. et al. 3D bioprinted silk fibroin hydrogels for tissue engineering. Nat Protoc. 2021;16:5484-532
141. Xue X, Zhang H, Liu H, Wang S, Li J, Zhou Q. et al. Rational Design of Multifunctional CuS Nanoparticle-PEG Composite Soft Hydrogel-Coated 3D Hard Polycaprolactone Scaffolds for Efficient Bone Regeneration. Adv Funct Mater. 2022;32:2202470
142. Lee JM, Sultan MT, Kim SH, Kumar V, Yeon YK, Lee OJ. et al. Artificial Auricular Cartilage Using Silk Fibroin and Polyvinyl Alcohol Hydrogel. Int J Mol Sci. 2017;18:1707
143. Wang K, Ma Q, Zhang Y-M, Han G-T, Qu C-X, Wang S-D. Preparation of bacterial cellulose/silk fibroin double-network hydrogel with high mechanical strength and biocompatibility for artificial cartilage. Cellulose. 2019;27:1845-52
144. Adali T, Kalkan R, Karimizarandi L. The chondrocyte cell proliferation of a chitosan/silk fibroin/egg shell membrane hydrogels. Int J Biol Macromol. 2019;124:541-7
145. Dong T, Mi R, Wu M, Zhong N, Zhao X, Chen X. et al. The regenerated silk fibroin hydrogel with designed architecture bioprinted by its microhydrogel. J Mater Chem B. 2019;7:4328-37
146. Dorishetty P, Balu R, Athukoralalage SS, Greaves TL, Mata J, de Campo L. et al. Tunable Biomimetic Hydrogels from Silk Fibroin and Nanocellulose. ACS Sustain Chem Eng. 2020;8:2375-89
147. Hu RZ, Zhang ZF, Yu BQ, Wang J, Yao XH, Chen T. et al. Natural phenolics and flavonoids modified the hierarchical cellular cellulose sponges for efficient water disinfection. Carbohydr Polym. 2022;296:119962
148. Zhang DY, Yang JX, Liu EJ, Hu RZ, Yao XH, Chen T. et al. Soft and elastic silver nanoparticle-cellulose sponge as fresh-keeping packaging to protect strawberries from physical damage and microbial invasion. Int J Biol Macromol. 2022;211:470-80
149. Hu R-Z, Zhang X-Q, Yao X-H, Yang J-X, Liu E-J, Chen T. et al. A bio-inspired dynamic filter with unidirectional channels based on cross-linked cellulose loading palladium nanoparticles for catalytic reduction of 4-nitrophenol. Ind Crops Prod. 2022;179:114690
150. Gan D, Jiang Y, Hu Y, Wang X, Wang Q, Wang K. et al. Mussel-inspired extracellular matrix-mimicking hydrogel scaffold with high cell affinity and immunomodulation ability for growth factor-free cartilage regeneration. J Orthop Translat. 2022;33:120-31
151. Yuan T, Shao Y, Zhou X, Liu Q, Zhu Z, Zhou B. et al. Highly Permeable DNA Supramolecular Hydrogel Promotes Neurogenesis and Functional Recovery after Completely Transected Spinal Cord Injury. Adv Mater. 2021;33:e2102428
152. Mao ZN, Bi XW, Wu CA, Zheng YF, Shu X, Wu SJ. et al. A Cell-Free Silk Fibroin Biomaterial Strategy Promotes In Situ Cartilage Regeneration Via Programmed Releases of Bioactive Molecules. Adv Healthc Mater. 2022;12:2201588
153. Cao Y, Wang BC. Biodegradation of Silk Biomaterials. Int J Mol Sci. 2009;10:1514-24
154. Haung SM, Lin YT, Liu SM, Chen JC, Chen WC. In Vitro Evaluation of a Composite Gelatin-Hyaluronic Acid-Alginate Porous Scaffold with Different Pore Distributions for Cartilage Regeneration. Gels. 2021;7:165
155. Singh YP, Bhardwaj N, Mandal BB. Potential of Agarose/Silk Fibroin Blended Hydrogel for in Vitro Cartilage Tissue Engineering. ACS Appl Mater Interfaces. 2016;8:21236-49
156. Izadifar Z, Chen X, Kulyk W. Strategic design and fabrication of engineered scaffolds for articular cartilage repair. J Funct Biomater. 2012;3:799-838
157. Guo J, Li C, Ling S, Huang W, Chen Y, Kaplan DL. Multiscale design and synthesis of biomimetic gradient protein/biosilica composites for interfacial tissue engineering. Biomaterials. 2017;145:44-55
158. Sawatjui N, Limpaiboon T, Schrobback K, Klein T. Biomimetic scaffolds and dynamic compression enhance the properties of chondrocyte- and MSC-based tissue-engineered cartilage. J Tissue Eng Regen Med. 2018;12:1220-9
159. Jess R, Ling T, Xiong Y, Wright CJ, Zhao F. Mechanical environment for in vitro cartilage tissue engineering assisted by in silico models. Biomater Transl. 2023;4:18-26
160. Huang X, Zhang M, Ming J, Ning X, Bai S. High-Strength and High-Toughness Silk Fibroin Hydrogels: A Strategy Using Dynamic Host-Guest Interactions. ACS Appl Bio Mater. 2020;3:7103-12
161. Shen C, Wang J, Li G, Hao S, Wu Y, Song P. et al. Boosting cartilage repair with silk fibroin-DNA hydrogel-based cartilage organoid precursor. Bioact Mater. 2024;35:429-44
162. Xu B, Ye J, Yuan FZ, Zhang JY, Chen YR, Fan BS. et al. Advances of Stem Cell-Laden Hydrogels With Biomimetic Microenvironment for Osteochondral Repair. Front Bioeng Biotechnol. 2020;8:247
163. Shen K, Duan A, Cheng J, Yuan T, Zhou J, Song H. et al. Exosomes derived from hypoxia preconditioned mesenchymal stem cells laden in a silk hydrogel promote cartilage regeneration via the miR-205-5p/PTEN/AKT pathway. Acta Biomater. 2022;143:173-88
164. Ni T, Liu M, Zhang Y, Cao Y, Pei R. 3D Bioprinting of Bone Marrow Mesenchymal Stem Cell-Laden Silk Fibroin Double Network Scaffolds for Cartilage Tissue Repair. Bioconjug Chem. 2020;31:1938-47
165. Calabrese R, Raia N, Huang W, Ghezzi CE, Simon M, Staii C. et al. Silk-ionomer and silk-tropoelastin hydrogels as charged three-dimensional culture platforms for the regulation of hMSC response. J Tissue Eng Regen Med. 2017;11:2549-64
166. Chen D, Chang P, Ding P, Liu S, Rao Q, Okoro OV. et al. MSCs-laden silk Fibroin/GelMA hydrogels with incorporation of platelet-rich plasma for chondrogenic construct. Heliyon. 2023;9:e14349
167. Zheng K, Zheng X, Yu M, He Y, Wu D. BMSCs-Seeded Interpenetrating Network GelMA/SF Composite Hydrogel for Articular Cartilage Repair. J Funct Biomater. 2023;14:39
168. Hong H, Seo YB, Kim DY, Lee JS, Lee YJ, Lee H. et al. Digital light processing 3D printed silk fibroin hydrogel for cartilage tissue engineering. Biomaterials. 2020;232:119679
169. Zorn AM, Wells JM. Vertebrate Endoderm Development and Organ Formation. Annu Rev Cell Dev Bi. 2009;25:221-51
170. Liu H, Zhang Q, Wang S, Weng W, Jing Y, Su J. Bacterial extracellular vesicles as bioactive nanocarriers for drug delivery: Advances and perspectives. Bioact Mater. 2021;14:169-81
171. Meng FY, Xue X, Yin ZF, Gao F, Wang XH, Geng Z. Research Progress of Exosomes in Bone Diseases: Mechanism, Diagnosis and Therapy. Front Bioeng Biotech. 2022;10:866627
172. Meng FY, Yin ZF, Ren XX, Geng Z, Su JC. Construction of Local Drug Delivery System on Titanium-Based Implants to Improve Osseointegration. Pharmaceutics. 2022;14:1069
173. Gao XJ, Dai QY, Yao LT, Dong H, Li QT, Cao XD. A medical adhesive used in a wet environment by blending tannic acid and silk fibroin. Biomater Sci-Uk. 2020;8:2694-701
174. Liu H, Li M, Zhang T, Liu X, Zhang H, Geng Z. et al. Engineered bacterial extracellular vesicles for osteoporosis therapy. Chem Eng J. 2022;450:138309
175. Zhang W, Zhang Y, Li X, Cao Z, Mo Q, Sheng R. et al. Multifunctional polyphenol-based silk hydrogel alleviates oxidative stress and enhances endogenous regeneration of osteochondral defects. Mater Today Bio. 2022;14:100251
176. Cao ZC, Wang HM, Chen JL, Zhang YA, Mo QY, Zhang P. et al. Silk-based hydrogel incorporated with metal-organic framework nanozymes for enhanced osteochondral regeneration. Bioact Mater. 2023;20:221-42
177. Chen PF, Zheng L, Wang YY, Tao M, Xie Z, Xia C. et al. Desktop-stereolithography 3D printing of a radially oriented extracellular matrix/mesenchymal stem cell exosome bioink for osteochondral defect regeneration. Theranostics. 2019;9:2439-59
178. Liu H, Zhang H, Han Y, Hu Y, Geng Z, Su J. Bacterial extracellular vesicles-based therapeutic strategies for bone and soft tissue tumors therapy. Theranostics. 2022;12:6576-94
179. Hu Y, Li X, Zhang Q, Gu Z, Luo Y, Guo J. et al. Exosome-guided bone targeted delivery of Antagomir-188 as an anabolic therapy for bone loss. Bioact Mater. 2021;6:2905-13
180. Zhang FX, Liu P, Ding W, Meng QB, Su DH, Zhang QC. et al. Injectable Mussel-Inspired highly adhesive hydrogel with exosomes for endogenous cell recruitment and cartilage defect regeneration. Biomaterials. 2021;278:121169
181. Jiang W, Xiang X, Song M, Shen J, Shi Z, Huang W. et al. An all-silk-derived bilayer hydrogel for osteochondral tissue engineering. Mater Today Bio. 2022;17:100485
182. Wu X, Zhou M, Jiang F, Yin S, Lin S, Yang G. et al. Marginal sealing around integral bilayer scaffolds for repairing osteochondral defects based on photocurable silk hydrogels. Bioact Mater. 2021;6:3976-86
183. He SJ, Fu XJ, Wang L, Xue YY, Zhou L, Qiao SG. et al. Self-Assemble Silk Fibroin Microcapsules for Cartilage Regeneration through Gene Delivery and Immune Regulation. Small. 2023;19:2302799
184. Chang L, Perez A. Ranking Peptide Binders by Affinity with AlphaFold. Angew Chem Int Ed Engl. 2023;62:e202213362
185. Jumper J, Evans R, Pritzel A, Green T, Figurnov M, Ronneberger O. et al. Highly accurate protein structure prediction with AlphaFold. Nature. 2021;596:583-9
186. Tang KY, Jiang L, Yeo JCC, Owh C, Ye E, Loh XJ. et al. Engineering luminescent pectin-based hydrogel for highly efficient multiple sensing. Int J Biol Macromol. 2021;166:869-75
187. Kambe Y, Yamaoka T. Initial immune response to a FRET-based MMP sensor-immobilized silk fibroin hydrogel in vivo. Acta Biomater. 2021;130:199-210
188. Ding J, Chen Z, Liu X, Tian Y, Jiang J, Qiao Z. et al. A mechanically adaptive hydrogel neural interface based on silk fibroin for high-efficiency neural activity recording. Mater Horiz. 2022;9:2215-25
189. Zhang H, Wang H, Wen B, Lu L, Zhao Y, Chai R. Ultrasound-Responsive Composited Conductive Silk Conduits for Peripheral Nerve Regeneration. Small Struct. 2023;4:2300045
190. Mahajan A, Singh A, Datta D, Katti DS. Bioinspired Injectable Hydrogels Dynamically Stiffen and Contract to Promote Mechanosensing-Mediated Chondrogenic Commitment of Stem Cells. ACS Appl Mater Interfaces. 2022;14:7531-50
191. Tao XY, Zhu KH, Chen HM, Ye SF, Cui PX, Dou LY. et al. Recyclable, anti-freezing and anti-drying silk fibroin-based hydrogels for ultrasensitive strain sensors and all-hydrogel-state super-capacitors. Mater Today Chem. 2023;32:101624
192. Haghighattalab M, Kajbafzadeh A, Baghani M, Gharehnazifam Z, Jobani BM, Baniassadi M. Silk Fibroin Hydrogel Reinforced With Magnetic Nanoparticles as an Intelligent Drug Delivery System for Sustained Drug Release. Front Bioeng Biotechnol. 2022;10:891166
193. Sun S, Liu H, Hu Y, Wang Y, Zhao M, Yuan Y. et al. Selection and identification of a novel ssDNA aptamer targeting human skeletal muscle. Bioact Mater. 2023;20:166-78
Author contact
![]() Corresponding authors: zdychemcom (Dongyang Zhou); dr.zhoufjcom (Fengjin Zhou); nanboshan1987com (Zhen Geng); drsujiacancom (Jiacan Su).
Corresponding authors: zdychemcom (Dongyang Zhou); dr.zhoufjcom (Fengjin Zhou); nanboshan1987com (Zhen Geng); drsujiacancom (Jiacan Su).
 Global reach, higher impact
Global reach, higher impact