13.3
Impact Factor
Theranostics 2022; 12(12):5564-5573. doi:10.7150/thno.74125 This issue Cite
Research Paper
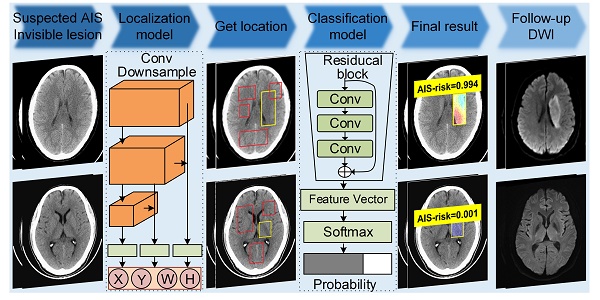
Identification of early invisible acute ischemic stroke in non-contrast computed tomography using two-stage deep-learning model
1. Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
2. Department of CT & MRI, The First Affiliated Hospital, College of Medicine, Shihezi University, Shihezi, China
3. Department of Artificial Intelligence, Julei Technology, Wuhan, China
4. Athinoula A. Martinos Center for Biomedical Imaging, Department of Radiology, Massachusetts General Hospital, Harvard Medical School, Charlestown, MA, USA
#These authors contributed equally to this work.
Abstract
Rationale: Although non-contrast computed tomography (NCCT) is the recommended examination for the suspected acute ischemic stroke (AIS), it cannot detect significant changes in the early infarction. We aimed to develop a deep-learning model to identify early invisible AIS in NCCT and evaluate its diagnostic performance and capacity for assisting radiologists in decision making.
Methods: In this multi-center, multi-manufacturer retrospective study, 1136 patients with suspected AIS but invisible lesions in NCCT were collected from two geographically distant institutions between May 2012 to May 2021. The AIS lesions were confirmed based on the follow-up diffusion-weighted imaging and clinical diagnosis. The deep-learning model was comprised of two deep convolutional neural networks to locate and classify. The performance of the model and radiologists was evaluated by the area under the receiver operator characteristic curve (AUC), sensitivity, specificity, and accuracy values with 95% confidence intervals. Delong's test was used to compare the AUC values, and a chi-squared test was used to evaluate the rate differences.
Results: 986 patients (728 AIS, median age, 55 years, interquartile range [IQR]: 47-65 years; 664 males) were assigned to the training and internal validation cohorts. 150 patients (74 AIS, median age, 63 years, IQR: 53-75 years; 100 males) were included as an external validation cohort. The AUCs of the model were 83.61% (sensitivity, 68.99%; specificity, 98.22%; and accuracy, 89.87%) and 76.32% (sensitivity, 62.99%; specificity, 89.65%; and accuracy, 88.61%) for the internal and external validation cohorts based on the slices. The AUC of the model was much higher than that of two experienced radiologists (65.52% and 59.48% in the internal validation cohort; 64.01% and 64.39% in external validation cohort; all P < 0.001). The accuracy of two radiologists increased from 62.00% and 58.67% to 92.00% and 84.67% when assisted by the model for patients in the external validation cohort.
Conclusions: This deep-learning model represents a breakthrough in solving the challenge that early invisible AIS lesions cannot be detected by NCCT. The model we developed in this study can screen early AIS and save more time. The radiologists assisted with the model can provide more effective guidance in making patients' treatment plan in clinic.
Keywords: artificial intelligence, deep-learning, acute ischemic stroke, non-contrast computed tomography, diagnosis
 Global reach, higher impact
Global reach, higher impact