13.3
Impact Factor
Theranostics 2021; 11(14):7018-7028. doi:10.7150/thno.59644 This issue Cite
Research Paper
Dynamic monitoring of circulating tumor DNA to predict prognosis and efficacy of adjuvant chemotherapy after resection of colorectal liver metastases
1. State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine, Sun Yat-sen University Cancer Center, Sun Yat-sen University, Guangzhou 510060, P. R. China.
2. Research Unit of Precision Diagnosis and Treatment for Gastrointestinal Cancer, Chinese Academy of Medical Sciences, Guangzhou 510060, P. R. China.
3. Department of Medical Oncology, Sun Yat-sen University Cancer Center, Guangzhou, People's Republic of China.
4. Department of Molecular Diagnostics, Sun Yat-sen University Cancer Center, Guangzhou, People's Republic of China.
5. HaploX Biotechnology, Co., Ltd., Shenzhen 518057, People's Republic of China.
6. Department of Hepatobiliary Surgery, Sun Yat-sen University Cancer Center, Guangzhou, People's Republic of China.
7. Department of Colorectal Surgery, Sun Yat-sen University Cancer Center, Guangzhou, People's Republic of China.
#These authors contributed equally to this study.
Abstract
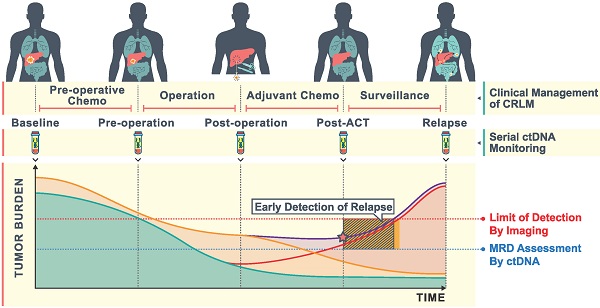
Rationale: Hepatectomy and adjuvant chemotherapy after resection of colorectal liver metastases (CRLM) may improve survival, however, patients which may benefit cannot currently be identified. Postoperative circulating tumor DNA (ctDNA) analysis can detect minimal residual disease (MRD) and predict the prognosis and efficacy of adjuvant chemotherapy. Our study aims to determine the impact of serial ctDNA analysis to predict the outcome among patients undergoing resection of CRLM.
Methods: Between May 2018 and October 2019, 91 CRLM patients were prospectively enrolled. Whole exome sequencing was performed in 50 primary and 48 metastatic liver tissues. Targeted sequencing of 451 cancer relevant genes was performed in 50 baseline plasma to determine plasma-tissue concordance. We prospectively investigated changes in the amount and constitution of ctDNA in 271 serial plasma samples taken at different time points (baseline, pre-operation, post-operation, post-operative adjuvant chemotherapy (post-ACT) and recurrence) during the treatment of CRLM.
Results: Detected molecular alterations were highly consistent among baseline ctDNA, primary and liver metastases tissue. Patients with a higher variant allele frequency (VAF) level at baseline ctDNA represent a higher tumor burden, and decreased ctDNA during pre-operative chemotherapy predicted better tumor response. Patients with detectable post-operative and post-ACT ctDNA were associated with significantly shorter recurrence-free survival (RFS). ROC analysis showed that post-ACT ctDNA status was superior to post-operative ctDNA status in predicting RFS with an AUROC of 0.79. A significant difference in overall recurrence rate was observed in patients with detectable vs undetectable levels of ctDNA after resection of CRLM (79.4% vs 41.7%) and after completion of adjuvant chemotherapy (77.3% vs 40.7%). During adjuvant chemotherapy, patients with decreased ctDNA VAF after adjuvant chemotherapy had a recurrence rate of 63.6%, compared to 92.3% in patients with increased ctDNA VAF.
Conclusions: We envision that dynamic ctDNA analysis, especially in a post-ACT setting, might be used to not only reflect MRD but also to determine rational personalized adjuvant therapy after the resection of CRLM.
Keywords: colorectal liver metastases, prognosis, ctDNA, next-generation sequencing, adjuvant chemotherapy
 Global reach, higher impact
Global reach, higher impact