13.3
Impact Factor
Theranostics 2020; 10(7):3254-3262. doi:10.7150/thno.39838 This issue Cite
Research Paper
Comparative prognostic implication of treatment response assessments in mCRPC: PERCIST 1.0, RECIST 1.1, and PSA response criteria
1. Division of Nuclear Medicine, Department of Radiology, Keck School of Medicine of USC, University of Southern California, Los Angeles, California
2. Department of Preventive Medicine, Keck School of Medicine of USC, University of Southern California, Los Angeles, California
3. Division of Oncology, Department of Medicine, Kenneth J. Norris Jr. Comprehensive Cancer Center, Keck School of Medicine of USC, University of Southern California, Los Angeles, California
Abstract
Accurate appraisal of treatment response in metastatic castrate-resistant prostate cancer (mCRPC) is challenging in view of remarkable tumor heterogeneity and the available choices among many established and novel therapeutic approaches. The purpose of this single-center prospective study was to evaluate the comparative prognostic utility of PERCIST 1.0 in predicting overall survival (OS) in patients with mCRPC compared to RECIST 1.1 and prostate-specific antigen (PSA)-based treatment response assessments.
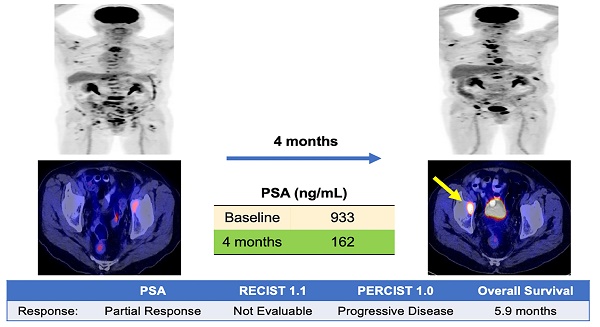
Methods: Patients with mCRPC were prospectively enrolled if they were beginning systemic medical therapy or transitioning to new systemic therapy after not responding to a prior treatment. All patients underwent a baseline 18F-fluorodeoxyglucose (FDG) positron emission tomography/ computed tomography (PET/CT) prior to the initiation of treatment and again 4 months after the start of therapy. Patients' responses to treatment at 4 months compared to baseline were evaluated with RECIST 1.1, PERCIST 1.0 and PSA response criteria. The associations between patients' response categories and OS were evaluated. OS was defined as the duration in time between the date of baseline PET/CT to death from any cause. Patients with different response status were compared with logrank tests. Survival probabilities were calculated using the Kaplan-Meier method.
Results: Patients with progressive disease by PSA response criteria at 4 months demonstrated significantly shorter OS (24-month OS probability: 18% ± 11%) compared to patients with stable disease, SD, (44% ± 19%, p=0.03) and complete response, CR, or partial response, PR, (53% ± 11%, p=0.03). RECIST 1.1 response criteria demonstrated a similar trend in OS, however no statistically significant differences were noted between patients with PD (25% ± 15%) compared to SD/non-CR, non-PD (54% ± 13%) and CR/PR (54% ± 14%) (p=0.13). PERCIST 1.0 criteria demonstrated significant differences in OS between responders, CMR/PMR (56% ± 12%), compared to SMD (38% ± 17%, p=0.03) and PMD (21% ± 10%, p=0.01). Patients with progressive disease by both PERICST 1.0 and PSA response criteria demonstrated significantly worse OS (24-month OS: 0%, 12-month OS: 31% ± 14%) compared to patients with progressive disease by either response criteria.
Conclusion: PERCIST 1.0 may provide significant prognostic information for patients with mCRPC undergoing systemic chemotherapy, particularly when incorporated with PSA treatment response criteria.
Keywords: 18F-FDG, PET/CT, Prostate, Cancer, Metastatic, Castrate-resistant
 Global reach, higher impact
Global reach, higher impact