13.3
Impact Factor
Theranostics 2019; 9(22):6646-6664. doi:10.7150/thno.33741 This issue Cite
Research Paper
Reversal of bleomycin-induced rat pulmonary fibrosis by a xenograft of human umbilical mesenchymal stem cells from Wharton's jelly
1. Division of Chest Medicine, Department of Internal Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, ROC
2. Department of Nursing, Shu-Zen Junior College of Medicine and Management, Kaohsiung, Taiwan, ROC
3. Institute of Anatomy and Cell Biology, School of Medicine, National Yang-Ming University, Taipei, Taiwan, ROC
4. Department of Obstetrics and Gynecology, Taipei Veterans General Hospital, Taipei, Taiwan, ROC
5. Department of Obstetrics and Gynecology, National Yang-Ming University, Taipei, Taiwan, ROC
6. Department of Nurse-Midwifery and Women Health, National Taipei University of Nursing and Health Sciences, Taipei, Taiwan, ROC
7. Department of Laboratory Medicine, Taipei Veterans General Hospital, Taipei, Taiwan, ROC
8. Department of Business Administration, Nan-Kai University of Technology, Nantou, Taiwan, ROC
9. School of Medicine, I-Shou University, Kaohsiung, Taiwan, ROC
10. Department of Medicine, Mackay Medical College, New Taipei, Taiwan, ROC
11. Trauma Center, Department of Surgery, Veterans General Hospital, Taipei, Taiwan, ROC
12. Division of General Surgery, Department of Surgery, Veterans General Hospital, Taipei, Taiwan, ROC.
13. Department of Critical Care Medicine, Veterans General Hospital, Taipei, Taiwan, ROC
14. Department of Anatomy and Cell Biology, School of Medicine, National Yang-Ming University, Taipei, Taiwan, ROC
Abstract
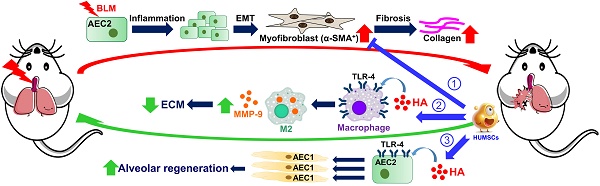
Pulmonary fibrosis (PF) is a progressive and irreversible condition with various causes, and no effective treatment has been found to rescue fibrotic lungs. Successful recovery from PF requires inhibiting inflammation, promoting collagen degradation and stimulating alveolar regeneration. Human umbilical mesenchymal stem cells (HUMSCs) not only regulate immune responses but also synthesize and release hyaluronan to improve lung regeneration. This study investigated the feasibility of HUMSC engraftment into rats with bleomycin (BLM)-induced PF to explore HUMSC therapeutic effects/outcomes.
Methods: A unique BLM-induced left-lung-dominated PF animal model was established. Rats were transplanted with low-dose (5×106) or high-dose (2.5×107) HUMSCs on Day 21 after BLM injection. Combinations in co-culture of pulmonary macrophages, fibroblasts, HUMSCs treated with BLM and the same conditions on alveolar epithelia versus HUMSCs were evaluated.
Results: Rats with high-dose HUMSC engraftment displayed significant recovery, including improved blood oxygen saturation levels and respiratory rates. High-dose HUMSC transplantation reversed alveolar injury, reduced cell infiltration and ameliorated collagen deposition. One month posttransplantation, HUMSCs in the rats' lungs remained viable and secreted cytokines without differentiating into alveolar or vascular epithelial cells. Moreover, HUMSCs decreased epithelial-mesenchymal transition in pulmonary inflammation, enhanced macrophage matrix-metallopeptidase-9 (MMP-9) expression for collagen degradation, and promoted toll-like receptor-4 (TLR-4) expression in the lung for alveolar regeneration. In coculture studies, HUMSCs elevated the MMP-9 level in pulmonary macrophages, released hyaluronan into the medium and stimulated the TLR-4 quantity in the alveolar epithelium.
Principal Conclusions: Transplanted HUMSCs exhibit long-term viability in rat lungs and can effectively reverse rat PF.
Keywords: Pulmonary fibrosis, Umbilical mesenchymal stem cells, Transplantation
 Global reach, higher impact
Global reach, higher impact