13.3
Impact Factor
Theranostics 2023; 13(12):4079-4101. doi:10.7150/thno.70372 This issue Cite
Review
Theranostics in the vasculature: bioeffects of ultrasound and microbubbles to induce vascular shutdown
1. Focused Ultrasound Foundation, Charlottesville, VA 22903, USA.
2. Department of Radiology, University of Virginia School of Medicine, Charlottesville, VA 22908, USA.
3. Ultrasound Neuroimaging and Therapy Lab, Fondazione IRCCS Istituto Neurologico C. Besta, Milan, Italy.
4. Department of Neurological Surgery, University of Virginia School of Medicine, Charlottesville, VA, USA.
5. Department of Biomedical Engineering, University of Virginia, Charlottesville, VA 22908, USA.
6. Cardiovascular Division, Department of Medicine, University of Virginia, Charlottesville, VA 22908, USA.
Abstract
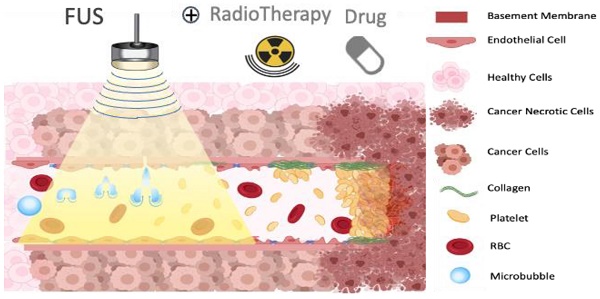
Ultrasound-triggered microbubbles destruction leading to vascular shutdown have resulted in preclinical studies in tumor growth delay or inhibition, lesion formation, radio-sensitization and modulation of the immune micro-environment. Antivascular ultrasound aims to be developed as a focal, targeted, non-invasive, mechanical and non-thermal treatment, alone or in combination with other treatments, and this review positions these treatments among the wider therapeutic ultrasound domain. Antivascular effects have been reported for a wide range of ultrasound exposure conditions, and evidence points to a prominent role of cavitation as the main mechanism. At relatively low peak negative acoustic pressure, predominantly non-inertial cavitation is most likely induced, while higher peak negative pressures lead to inertial cavitation and bubbles collapse. Resulting bioeffects start with inflammation and/or loose opening of the endothelial lining of the vessel. The latter causes vascular access of tissue factor, leading to platelet aggregation, and consequent clotting. Alternatively, endothelium damage exposes subendothelial collagen layer, leading to rapid adhesion and aggregation of platelets and clotting. In a pilot clinical trial, a prevalence of tumor response was observed in patients receiving ultrasound-triggered microbubble destruction along with transarterial radioembolization. Two ongoing clinical trials are assessing the effectiveness of ultrasound-stimulated microbubble treatment to enhance radiation effects in cancer patients. Clinical translation of antivascular ultrasound/microbubble approach may thus be forthcoming.
Keywords: antivascular therapy, ultrasound, cavitation, microbubbles, drug delivery, tumor therapy
 Global reach, higher impact
Global reach, higher impact