13.3
Impact Factor
Theranostics 2023; 13(5):1584-1593. doi:10.7150/thno.81789 This issue Cite
Research Paper
Development and validation of a nonenhanced CT based radiomics model to detect brown adipose tissue
1. Department of Nuclear Medicine, Jinling Hospital, Medical School of Nanjing University, Nanjing 210002, China.
2. Department of Radiology, Jinling Hospital, Medical School of Nanjing University, Nanjing 210002, China.
3. Division of Cardiovascular Imaging, Department of Radiology and Radiological Science, Medical University of South Carolina, 25 Courtenay Dr, Charleston, SC, 29425, USA.
4. Deepwise AI Lab, Beijing Deepwise & League of PhD Technology Co.Ltd, China.
5. Department of Radiology, Qinhuai Medical District, Jinling Hospital, Medical School of Nanjing University, Nanjing 210002, China.
Abstract
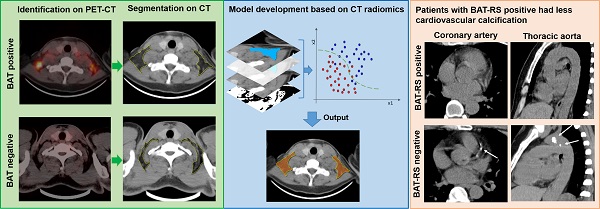
Purpose: It has been reported that brown adipose tissue (BAT) has a protective effect regarding cardiovascular disease. Positron emission tomography-computed tomography (PET-CT) is the reference method for detecting active BAT; however, it is not feasible to screen for BAT due to the required radionuclides and high-cost. The purpose of this study is to develop and validate a nonenhanced CT based radiomics model to detect BAT and to explore the relationship between CT radiomics derived BAT and cardiovascular calcification.
Patients and methods: 146 patients undergoing 18F-FDG PET-CT were retrospectively included from two centers for model development (n = 86) and external validation (n = 60). The data for the model development were randomly divided into a training cohort and an internal validation cohort with a 7:3 ratio, while the external validation data were divided 1:1 into a propensity score matching (PSM) cohort and a randomly sex matched cohort. Radiomics features of BAT and non-BAT depots were extracted from regions of interest (ROI) on nonenhanced CT corresponding to PET studies. Inter-class correlation coefficient (ICC) and Pearson's correlation analysis were performed to select radiomics features with high consistency. Next, least absolute shrinkage and selection operator (LASSO) with linear regression model was used to select radiomics features for model construction. Support vector machine (SVM) was used to develop the model and a radiomics score (RS) was calculated for each depot. The diagnostic performance of the radiomics model was evaluated both on a per-depot and per-patient basis by calculating the area under the receiver operating characteristic curve (AUROC). We further divided patients into BAT-RS group and non-BAT-RS group based on radiomics score and compared their cardiovascular calcification by calculating calcium volume and score.
Results: A total of 22 radiomics features were selected for model construction. On a per-depot basis, the AUROCs were 0.87 (95% CI: 0.83-0.9), 0.85 (95% CI: 0.79-0.90), 0.72 (95% CI: 0.67-0.77) and 0.74 (95% CI: 0.69-0.79) for detecting BAT in the training, internal validation, external validation 1 and external validation 2 cohorts, respectively. On a per-patient basis, the radiomics model had high AUROCs of 0.91 (95% CI: 0.84-0.98), 0.77 (95% CI: 0.61-0.92) and 0.85 (95% CI: 0.72-0.98) in the training, external validation 1 and external validation 2 cohorts, respectively. When grouping based on the radiomics model, the BAT-RS group had lower odds of coronary artery calcium (CAC) and thoracic aorta calcium (TAC) compared with the non-BAT-RS group (CAC: 2.8% vs. 20.3%, p = 0.001; TAC: 19.4% vs. 39.2%, p = 0.009). The BAT-RS group had less CAC volume (4.1 ± 4.0 mm3 vs. 147.4 ± 274.3 mm3; p = 0.001), CAC score (2.8 ± 3.0 vs. 169.1 ± 311.5; p = 0.001), TAC volume (301.4 ± 450.2 mm3 vs. 635.3 ± 1100.7 mm3; p = 0.007) and TAC score (496.2 ± 132.6 vs. 749.2 ± 1297.3; p = 0.007) than the non-BAT-RS group.
Conclusion: We developed and validated a nonenhanced CT based reliable radiomics model for detecting BAT with PET-CT findings as reference standard. Radiomics signatures from nonenhanced CT can reliably detect BAT and have promising potential to be used in routine clinical settings. Importantly, our study showed that patients with BAT had less cardiovascular calcification.
Keywords: Brown adipose tissues, radiomics, PET-CT, cardiovascular calcification
 Global reach, higher impact
Global reach, higher impact