13.3
Impact Factor
Theranostics 2020; 10(21):9779-9788. doi:10.7150/thno.49671 This issue Cite
Research Paper
Prediction of clinically relevant Pancreatico-enteric Anastomotic Fistulas after Pancreatoduodenectomy using deep learning of Preoperative Computed Tomography
1. Beijing Advanced Innovation Center for Big Data-Based Precision Medicine, School of Medicine, Beihang University, Beijing, China, 100191.
2. Department of Radiology, Shengjing Hospital of China Medical University, Shenyang, China.
3. Department of Pancreato-thyroidic Surgery, Shengjing Hospital of China Medical University, Shenyang, China.
4. Department of Pathology, Shengjing Hospital of China Medical University, Shenyang, China.
5. Department of Radiology, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center of Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, PR China.
6. Department of Radiology, Guangdong General Hospital, Guangdong Academy of Medical Sciences, 106 Zhongshan Er Road, Guangzhou 510080, China.
7. Key Laboratory of Molecular Imaging, Chinese Academy of Sciences, Beijing, China, 100190.
Abstract
Rationale: Clinically relevant postoperative pancreatic fistula (CR-POPF) is among the most formidable complications after pancreatoduodenectomy (PD), heightening morbidity/mortality rates. Fistula Risk Score (FRS) is a well-developed predictor, but it is an intraoperative predictor and quantifies >50% patients as intermediate risk. Therefore, an accurate and easy-to-use preoperative index is desired. Herein, we test the hypothesis that quantitative analysis of contrast-enhanced computed tomography (CE-CT) with deep learning could predict CR-POPFs.
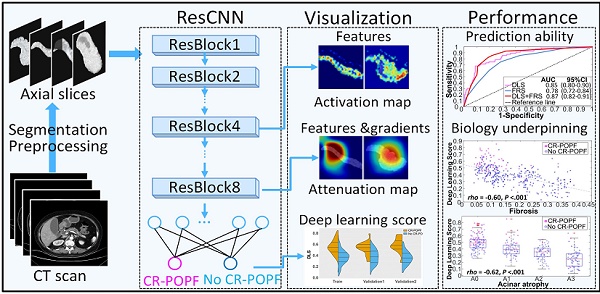
Methods: A group of 513 patients underwent pancreatico-enteric anastomosis after PD at three institutions between 2006 and 2019 was retrospectively collected, and formed a training (70%) and a validation dataset (30%) randomly. A convolutional neural network was trained and generated a deep-learning score (DLS) to identify the patients with higher risk of CR-POPF preoperatively using CE-CT images, which was further externally tested in a prospective cohort collected from August 2018 to June 2019 at the fourth institution. The biological underpinnings of DLS were assessed using histomorphological data by multivariate linear regression analysis.
Results: CR-POPFs developed in 95 patients (16.3%) in total. Compared to FRS, the DLS offered significantly greater predictability in training (AUC:0.85 [95% CI, 0.80-0.90] vs. 0.78 [95% CI, 0.72-0.84]; P = 0.03), validation (0.81 [95% CI, 0.72-0.89] vs. 0.76 [95% CI, 0.66-0.84], P = 0.05) and test (0.89 [95% CI, 0.79-0.96] vs. 0.73 [95% CI, 0.61-0.83], P < 0.001) cohorts. Especially in the challenging patients of intermediate risk (FRS: 3-6), the DLS showed significantly higher accuracy (training: 79.9% vs. 61.5% [P = 0.005]; validation: 70.3% vs. 56.3% [P = 0.04]; test: 92.1% vs. 65.8% [P = 0.013]). Additionally, DLS was independently associated with pancreatic fibrosis (coefficients: -0.167), main pancreatic duct (coefficients: -0.445) and remnant volume (coefficients: 0.138) in multivariate linear regression analysis (r2 = 0.512, P < 0.001). The user satisfaction score in the test cohort was 4 out of 5.
Conclusions: Preoperative CT based deep-learning model provides a promising novel method for predicting CR-POPF occurrences after PD, especially at intermediate FRS risk level. This has a potential to be integrated into radiologic reporting system or incorporated into surgical planning software to accommodate the preferences of surgeons to optimize preoperative strategies, intraoperative decision-making, and even postoperative care.
Keywords: Pancreatic fistula, fistula risk score, pancreatoduodenectomy, computed tomography (CT), deep learning
 Global reach, higher impact
Global reach, higher impact