13.3
Impact Factor
Theranostics 2020; 10(17):7812-7820. doi:10.7150/thno.47251 This issue Cite
Research Paper
Analysis of PSMA expression and outcome in patients with advanced Prostate Cancer receiving 177Lu-PSMA-617 Radioligand Therapy
1. Department of Nuclear Medicine, University Hospital Münster, Münster, Germany.
2. Department of Nuclear Medicine, University Hospital Essen, Essen, Germany.
3. German Cancer Consortium (DKTK).
4. West German Cancer Center.
5. Department of Urology, University Hospital Münster, Münster, Germany.
6. Division of Radiology, German Cancer Research Center, Heidelberg, Germany.
Abstract
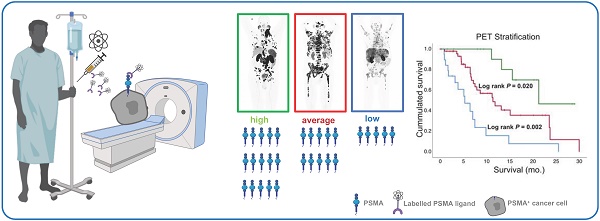
Rationale: PSMA-PET-CT enables measuring molecular expression of prostate-specific membrane antigen (PSMA) in vivo, which is the target molecule of 177Lu-PSMA-617 (Lu-PSMA) therapy. However, the correlation of PSMA expression and overall survival (OS) in patients treated with Lu-PSMA therapy is currently unclear; especially with regard to coexistence of high and low PSMA expressing metastases. To this end, this retrospective single arm study elucidates the correlation of PSMA expression and overall survival in patients treated with Lu-PSMA therapy. Additionally, PET based criteria to define low PSMA expression were explored.
Methods: Eighty-five patients referred to Lu-PSMA therapy were included in the analysis. Pretherapeutic 68Ga-PSMA-PET-CT scans were available for all patients. SUVmax of the highest PSMA expressing metastasis (PSMAmax), SUVmax of the lowest PSMA expressing metastasis (PSMAmin), and average SUVmax of all metastases (PSMAaverage) amongst other PET parameters were measured for each patient. A log-rank cutoff-finder was used to determine low (lowPSMAaverage) and high (highPSMAaverage) average PSMA expression as well as low (lowPSMAmin) and high (highPSMAmin) minimal PSMA expression.
Results: PSMAaverage was a significant prognosticator of overall survival in contrast to PSMAmax (HR: 0.959; p = 0.047 vs. HR: 0.992; p = 0.231). Optimal log rank cut-offs were: PSMAaverage = 14.3; PSMAmin = 10.2. Patients with low average PSMA expression (lowPSMAaverage) had significantly shorter survival compared to those with high average expression (highPSMAaverage) (5.3 vs. 15.1 months; p < 0.001; HR: 3.738, 95%CI = 1.953-7.154; p < 0.001). Patients with low PSMA expressing metastases (lowPSMAmin) had shorter survival compared to those without a low PSMA expressing metastasis (highPSMAmin) (p = 0.003; 7.9 months vs. 21.3; HR: 4.303, 95%CI = 1.521-12.178; p = 0.006). Patients that were classified as highPSMAaverage but with lowPSMAmin had an intermediate overall survival (11.4 months; longer compared to lowPSMAaverage, 5.3 months, p = 0.002; but shorter compared to highPSMAmin, 21.3 months, p = 0.02).
Conclusion: Low average PSMA expression is a negative prognosticator of overall survival. Absence of low PSMA expressing metastases is associated with best overall survival and the maximum PSMA expression seems not suited to prognosticate overall survival. Low PSMA expression might therefore be a negative prognosticator for the outcome of patients treated with Lu-PSMA therapy. Future studies are warranted to elucidate the degree of low PSMA expression tolerable for Lu-PSMA therapy.
Keywords: PSMA radioligand therapy, PSMA PET, prostate cancer, prognosticator
 Global reach, higher impact
Global reach, higher impact