13.3
Impact Factor
Theranostics 2020; 10(16):7211-7230. doi:10.7150/thno.47281 This issue Cite
Research Paper
Ultrafast three-dimensional microbubble imaging in vivo predicts tissue damage volume distributions during nonthermal brain ablation
1. Physical Sciences Platform, Sunnybrook Research Institute, Toronto, Ontario, Canada.
2. Department of Medical Biophysics, University of Toronto, Toronto, Ontario, Canada.
3. Institute of Biomaterials and Biomedical Engineering, University of Toronto, Toronto, Ontario, Canada.
Abstract
Transcranial magnetic resonance imaging (MRI)-guided focused ultrasound (FUS) thermal ablation is under clinical investigation for non-invasive neurosurgery, though its use is restricted to central brain targets due primarily to skull heating effects. The combination of FUS and contrast agent microbubbles greatly reduces the ultrasound exposure levels needed to ablate brain tissue and may help facilitate the use of transcranial FUS ablation throughout the brain. However, sources of variability exist during microbubble-mediated FUS procedures that necessitate the continued development of systems and methods for online treatment monitoring and control, to ensure that excessive and/or off-target bioeffects are not induced from the exposures.
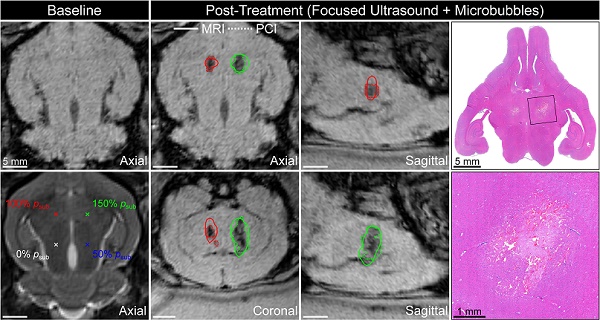
Methods: Megahertz-rate three-dimensional (3D) microbubble imaging in vivo was performed during nonthermal ablation in rabbit brain using a clinical-scale prototype transmit/receive hemispherical phased array system.
Results: In-vivo volumetric acoustic imaging over microsecond timescales uncovered spatiotemporal microbubble dynamics hidden by conventional whole-burst temporal averaging. Sonication-aggregate ultrafast 3D source field intensity data were predictive of microbubble-mediated tissue damage volume distributions measured post-treatment using MRI and confirmed via histopathology. Temporal under-sampling of acoustic emissions, which is common practice in the field, was found to impede performance and highlighted the importance of capturing adequate data for treatment monitoring and control purposes.
Conclusion: The predictive capability of ultrafast 3D microbubble imaging, reported here for the first time, will enable future microbubble-mediated FUS treatments with unparalleled precision and accuracy, and will accelerate the clinical translation of nonthermal tissue ablation procedures both in the brain and throughout the body.
Keywords: image-guided therapy, focused ultrasound, microbubble contrast agents, nonthermal ablation, ultrafast 3D acoustic imaging
 Global reach, higher impact
Global reach, higher impact