13.3
Impact Factor
Theranostics 2020; 10(3):1074-1089. doi:10.7150/thno.37931 This issue Cite
Research Paper
Modulating the cobalt dose range to manipulate multisystem cooperation in bone environment: a strategy to resolve the controversies about cobalt use for orthopedic applications
1. Institute of Stomatology and Department of Oral Implantology, Guanghua School of Stomatology, Hospital of Stomatology, Sun Yat-sen University and Guangdong Provincial Key Laboratory of Stomatology, Guangzhou 510055, China;
2. Zhujiang New Town Clinic, Guanghua School of Stomatology, Hospital of Stomatology, Sun Yat-sen University and Guangdong Provincial Key Laboratory of Stomatology, Guangzhou 510055, China.
*These authors contributed equally to this work.
Abstract
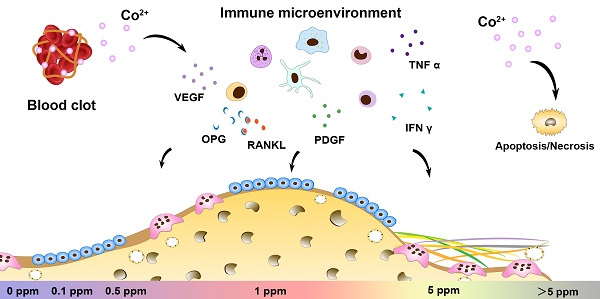
The paradoxical effect of cobalt on biological processes has aroused controversy regarding the application of cobalt-based biomaterials in bone regeneration. Tuning the dose range of cobalt ions may be a valid strategy to resolve the controversies about cobalt use for orthopedic applications. Recent progress in bone biology has highlighted the effects of multisystem cooperation (especially of osteoimmune, skeletal, and vascular systems) on bone dynamics. Before the application of this dose-tuning strategy, a deeper understanding of its dose-dependent effect on the cooperation of osteoimmune, skeletal, and vascular systems is needed. However, due to the difficulties with investigating the interaction of multiple systems in vitro, the multimodal effects of cobalt on bone homeostasis were investigated here, in an in vivo scenario.
Methods: In vitro CCK8 assay and cytoskeletal staining were preformed to detecte the cell cytotoxic reaction in response to 0.1-100 ppm cobalt stimulation. Blood clot containing 0.1 to 5 ppm of cobalt were implanted in the rat calvarium defect. The gene profile of osteoimmune, skeletal, and vascular system as well as the systemic toxicity were evaluated via RT-qPCR, histological analysis and inductively coupled plasma mass spectrometry. The bone regeneration, osteoclastogenesis and vascularization were assessed by micro-ct and histological analysis.
Results: Cobalt concentration below 5 ppm did not cause cell toxicity in vitro. No systemic toxicity was observed in vivo at 0.1-5 ppm cobalt concentration. It was found that the early cytokine profiles of the multiple interacting systems were different in response to different cobalt doses. Most of the anti-inflammatory, osteogenic, and proangiogenic factors were upregulated in the 1 ppm cobalt group at the early stage. In the late stage, the 1ppm group was most superior in bone regenerative effect while the 5 ppm group displayed the strongest osteoclastogenesis activity.
Conclusions: The 1 ppm concentration of cobalt yielded the most favorable cooperation of the osteoimmune, skeletal, and vascular systems and subsequently optimal bone regeneration outcomes. Tuning the cobalt dose range to manipulate the cooperation of osteoimmune, skeletal, and vascular systems could be a promising and valuable strategy to prevent paradoxical effects of cobalt while preserving its beneficial effects.
Keywords: cobalt, systems immunology, osteoimmunomodulation, angiogenesis, bone regeneration.
 Global reach, higher impact
Global reach, higher impact