13.3
Impact Factor
Theranostics 2018; 8(21):5929-5944. doi:10.7150/thno.28029 This issue Cite
Research Paper
Targeted homing of CCR2-overexpressing mesenchymal stromal cells to ischemic brain enhances post-stroke recovery partially through PRDX4-mediated blood-brain barrier preservation
1. Department of Neurology, The Third Affiliated Hospital, Sun Yat-Sen University, No. 600 Tianhe Road, Guangzhou, China, 510630
2. Center for Stem Cell Biology and Tissue Engineering, Key Laboratory for Stem Cells and Tissue Engineering, Ministry of Education, Sun Yat-Sen University, Guangzhou, China, 510080
3. Department of Hepatic Surgery and Liver Transplantation Center, The Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-Sen University, Guangzhou, China, 510630
4. Department of Rehabilitation Medicine, The Third Affiliated Hospital, Sun Yat-Sen University, Guangzhou, 510630, China.
5. Department of Surgery Intensive Care Unit, The Third Affiliated Hospital, Sun Yat-Sen University, Guangzhou, 510630, China.
6. Department of Neurology, The Fifth Affiliated Hospital, Sun Yat-Sen University, No. 52 Mei Hua East Road, Zhuhai, China, 519000
7. Department of Medical Ultrasonic, Third Affiliated Hospital, Sun Yat-Sen University, Guangzhou 510630, China.
8. Department of Biochemistry, Zhongshan School of Medicine, Sun Yat-Sen University, Guangzhou, China, 510080
*Co-first author
Abstract
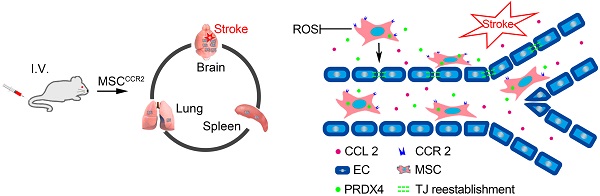
Rationale: Mesenchymal stromal cells (MSCs) are emerging as a novel therapeutic strategy for the acute ischemic stroke (AIS). However, the poor targeted migration and low engraftment in ischemic lesions restrict their treatment efficacy. The ischemic brain lesions express a specific chemokine profile, while cultured MSCs lack the set of corresponding receptors. Thus, we hypothesize that overexpression of certain chemokine receptor might help in MSCs homing and improve therapeutic efficacy. Methods: Using the middle cerebral artery occlusion (MCAO) model of ischemic stroke, we identified that CCL2 is one of the most highly expressed chemokines in the ipsilateral hemisphere. Then, we genetically transduced the corresponding receptor, CCR2 to the MSCs and quantified the cell retention of MSCCCR2 compared to the MSCdtomato control. Results: MSCCCR2 exhibited significantly enhanced migration to the ischemic lesions and improved the neurological outcomes. Brain edema and blood-brain barrier (BBB) leakage levels were also found to be much lower in the MSCCCR2-treated rats than the MSCdtomato group. Moreover, this BBB protection led to reduced inflammation infiltration and reactive oxygen species (ROS) generation. Similar results were also confirmed using the in vitro BBB model. Furthermore, genome-wide RNA sequencing (RNA-seq) analysis revealed that peroxiredoxin4 (PRDX4) was highly expressed in MSCs, which mainly contributed to their antioxidant impacts on MCAO rats and oxygen-glucose deprivation (OGD)-treated endothelium. Conclusion: Taken together, this study suggests that overexpression of CCR2 on MSCs enhances their targeted migration to the ischemic hemisphere and improves the therapeutic outcomes, which is attributed to the PRDX4-mediated BBB preservation.
Keywords: Mesenchymal stromal cells, CCL2/CCR2, blood brain barrier, endothelium, PRDX4
 Global reach, higher impact
Global reach, higher impact