13.3
Impact Factor
Theranostics 2018; 8(12):3392-3399. doi:10.7150/thno.24083 This issue Cite
Research Paper
Comparison of Burnet's clonal selection theory with tumor cell-clone development
Institute of Laboratory Medicine and Pathobiochemistry, Molecular Diagnostics, University Hospital of the Universities of Giessen and Marburg UKGM, Justus Liebig University, Giessen, Giessen Germany
Received 2017-11-29; Accepted 2018-4-10; Published 2018-5-23
Abstract
Increasing evidence has shown that Darwin's theory of evolution provides vital insights into the emergence and etiology of different types of cancer. On a microscopic scale, cancer stem cells meet the conditions for the Darwinian process of natural selection. In particular, cancer stem cells undergo cell reproduction characterized by the emergence of heritable variability that promotes replication and cell survival.
Methods: Evidence from previous studies was gathered to compare Burnet's clonal selection theory with the tumor evolution theory.
Results: The findings show that the Darwinian theory offers a general framework for understanding fundamental aspects of cancer. As fundamental theoretical frameworks, Burnet's clonal selection theory and the tumor evolution theory can be used to explain cancer cell evolution and identify the beneficial adaptations that contribute to cell survival in tissue landscapes and tissue ecosystems.
Conclusions: In conclusion, this study shows that both Burnet's clonal selection theory and the tumor evolution theory postulate that cancer cells in tissue ecosystems evolve through reiterative processes, such as clonal expansion, clonal selection, and genetic diversification. Therefore, both theories provide insights into the complexities and dynamics of cancer, including its development and progression. Finally, we take into account the occurrence of biologic variation in both tumor cells and lymphocytes. It is important to note that the presence of lymphocyte variations appears to be advantageous in the framework of tumor defense but also dangerous within the framework of autoimmune disease development.
Keywords: Burnet, evolution, tumor development, lymphocyte proliferation, cell clone theory
Introduction
Cancer remains a leading cause of mortality and poor health worldwide [1, 2]. Despite the enormous amount of money, resources, and effort expended in the last two decades, successful control and eradication of the disease have remained elusive [3, 4]. Furthermore, an increasing worldwide prevalence of various risk factors, such as smoking, obesity, and physical inactivity, that increase the likelihood of cancer development has been revealed over the last decade [5, 6, 7]. However, our understanding of cancer genetics and biology has improved significantly. Moreover, knowledge regarding the complexity of cancer and its evolutionary characteristics provides a reliable basis and opportunities for developing interventions and therapies to manage and control the disease [8]. Greaves noted that scientists such as Peter Nowell and Macfarlane Burnet have developed groundbreaking theories describing cancer progression and development as evolutionary processes driven by somatic cell mutations and subclonal selection [9]. Their unique theories have explicit parallels to Darwinian natural selection, in which cancer is viewed as an asexual process that produces single mutated cells and quasispecies [9, 10]. Modern cancer genomics and biology have validated the concept that cancer development is a complex, adaptive, and Darwinian process.
Cancer development occurs within a tissue ecosystem that evolves to integrate and optimize multicellular functions while simultaneously controlling renegade clonal expansion [11, 12, 13]. Tissues in the tumor microenvironment provide the basis and context for cancer development and cancer cell evolution. In addition, the protracted time that typically precedes the clinical emergence of different cancer types and the mutational complexity reflect the random and sequential search for phenotypic solutions to constraints in the microenvironment, such as telomere stabilization, resource limitations, and self-renewal ability [11, 14].
Furthermore, tumor microenvironment factors, such as resource restriction, limit tumor size at all stages of cancer progression [15, 16, 17]. Therefore, the selection of tumors in the case of organisms occurs by intense competition for resources and space. The general application of evolutionary ecology and biology principles will improve our understanding of cancer development as an evolutionary process [15] and will inform the dynamics and complexities of cancer treatment. This study compares Burnet's clonal selection theory with the tumor evolution theory to identify useful information and insights on the complexities and dynamics of cancer development and progression.
Methods
The objective of this paper was to explore the evolutionary processes associated with cancer development and progression. To achieve this objective and to contribute to the understanding of cancer, a systematic review of peer-reviewed journal articles on Burnet's clonal selection theory and the clonal tumor evolution theory was conducted. The articles were obtained from various electronic databases, including PubMed. The process of collecting evidence began with a careful search for articles from selected electronic databases. The search terms and phrases included “Burnet's clonal selection theory,” “clonal selection theory,” “clonal tumor evolution theory,” “Darwinistic selection in cancer development,” “Darwinistic selection and hematopoietic lineage,” “clonal evolution in cancer,” and “tumor evolution theory.” The intention was to locate reliable articles that are relevant to the study objective. Notably, the search was limited only to English articles published between 2013 and 2017 to ensure that the conclusions of this study were based on current research.
An initial search of the selected databases and cross-references identified 229 articles related to cancer development as an evolutionary process. From this initial list of peer-reviewed articles, the researcher excluded sources that were duplicates, those that did not address Burnet's clonal selection theory and the clonal tumor evolution theory, and sources that were beyond the scope of this study. Study selection was also restricted to the most relevant and recent articles related to the topic of this study. At the end of the screening process, 50 articles remained. An additional 20 articles were selected by performing a manual search of relevant studies from the reference lists of the 50 included articles. All 70 articles were subjected to a full-text review, wherein the researcher analyzed the aims, methodologies, results, and conclusions of each study. In addition, this study reviewed the limitations of each study to determine how they might affect the conclusions of this systematic review.
Results and Discussion
Clonal dynamics and mutational drivers in cancer development
Greaves stated that cancer is a multifaceted healthcare problem that affects every area of clinical practice [9]. Therefore, efforts to develop and use effective intervention measures, such as chemotherapy, to manage the condition are constantly underway to help patients regain their former state of health [9]. A review of previous studies revealed that one of the greatest challenges for the management and therapeutic control of cancer is the issue of dynamic genetic diversity and epigenetic plasticity among cancer patients [18, 19]. Classical evolution theories, such as the Darwinian theory of evolution, have been used to explore and explain the epigenetic plasticity and genetic diversity associated with various types of cancer [9]. Darwin's evolution theory proposes a fundamental principle of natural selection for the fittest organisms and variants [20, 21, 22].
Greaves states that Darwin's evolution theory holds that natural selection favors organisms and variants that fortuitously develop and express traits that thwart or complement contemporary selective constraints or pressures [9, 23]. Cancer is viewed as a clear illustration of the Darwinian system and process. Moreover, mutations at the DNA sequence level among cancer patients are associated with error-prone repair processes and genotoxic exposure, such as exposure to chemotherapeutic agents, cigarette-related carcinogens, and UV light, which can cause cancer [9, 24, 25]. Adaptive mutations in the tumor environment reflect the process of gaining fitness traits, allowing cancer cells to survive and multiply [26, 27]. The Darwinistic selection process in cancer pathogenesis supports the generation of species and facilitates the formation of mutant subsets in hematopoietic lineages, such as lymphocytes [27, 28, 29]. Moreover, this process contributes to the emergence of enhanced receptors for survival and to better control of suicide mechanisms in the case of lymphocyte development [29, 30]. In this regard, the development and progression of cancer correspond to the natural selection of the fittest organisms in an ecosystem.
Burnet's clonal selection theory
Burnet's clonal selection theory is a scientific theory that explains and demonstrates the functions of lymphocytes and their responses to antigens that attack the body [31]. In other words, this theory introduced and promoted by Frank Macfarlane Burnet describes the formation process of diverse antibodies in the initial stages of the immune response [31]. Burnet's clonal selection theory has been featured extensively in studies that have sought to investigate the immunological tolerance of cancer cells due to clonal selection. According to Andor, Maley, and Hanlee, clonal selection refers to the ability of an organism to tolerate and withstand the introduction of cells without initiating an immune response as long as the cells are introduced in the early stages of the organism's development [31].
Several types of lymphocytes exist in the immune system. Some of these cells are tolerant to self-tissues, while others are intolerant to self-tissues. However, notably, only cells that tolerate self-tissues survive the embryonic stage of development. In addition, the introduction of a nonself-tissue leads to the development of lymphocytes that include nonself-tissues as part of their self-tissues [32, 33]. Frank Macfarlane Burnet proposed the clonal selection theory to explain and examine the functions of lymphocytes in the immune system and to assess how they respond to specific antigens that invade the body [32, 33]. Moreover, the theory provides a basis for understanding how the immune system responds to infections and how B and T lymphocytes are usually selected to destroy particular antigens [32, 33].
Burnet's clonal selection theory postulates that in a preexisting group or population of lymphocytes, a particular antigen can activate only its specific counter cell, inducing that specific cell to multiply and create clones for antibody production [34]. This activation occurs in secondary lymphoid organs, such as the lymph nodes and spleen [34]. In other words, Burnet's clonal selection theory explains the mechanism that leads to diversity in antibody specificity. Burnet's hypothesis further states that lymphocytes can correspond to all antigenic determinants of the biological materials in the body with varying degrees of precision. Greaves states that when antigens enter tissue fluids or the blood, they attach to the surfaces of any lymphocytes with reactive sites that correspond to its antigenic determinant [9]. The cell is then activated and undergoes proliferation, resulting in the production of a wide range of descendants [9, 34]. The clones, or descendants, have the capacity to activate the release of lymphocytes and a soluble antibody that can perform the same immune function as its parental cell [9, 32, 33, 34].
A systematic review by Rose reported that the success of adaptive immunity according to Burnet's clonal selection theory is based on the assumption that the entire range of receptors in both T and B lymphocytes is sufficient to accurately and precisely recognize any pathogen [35]. The author also noted that an antigen selects, binds, and activates the appropriate lymphocytes to replicate serially and produce lymphocyte clones with the same antigen-specific receptors [35]. The clonal selection theory predicts that any premature exposure to a similar antigen will lead to lymphocyte death rather than the expected proliferation [36, 37, 38]. For example, if a similar antigen is encountered during the initial stages of lymphocyte generation, when antigen specificity is first conferred, cell death and clonal deletion will ensue [35, 39, 40]. According to Rose, Burnet believed that negative selection was the mechanism that caused the elimination and death of self-directed lymphocyte clones during development and adaptive immune responses [35].
Notably, clonal deletion can occur during the initial differentiation of antigen-specific T or B lymphocytes or later in peripheral sites [35]. For antigen-specific T cells, differentiation occurs in the thymus, where T cells with antigen-specific receptors encounter their respective antigens in the thymic medulla. When the thymic medullary cells present a specific antigen epitope, the T cells experience apoptotic cell death [41, 42, 43]. Regarding Burnet's clonal selection theory, these T cells produce no progeny. Therefore, the host will not be able to respond and will be considered tolerant to a given antigen [35]. Apoptosis is viewed as one of the main obstacles that tumor cells must circumnavigate to proliferate and survive under the stressful conditions of the tumor microenvironment [35, 44, 45]. Notably, cancer is viewed by researchers such as Dawson, Rosenfeld, and Caldas and de Bruin as a condition that results from consecutive genetic changes transforming normal cells into malignant cells [46, 47]. Evasion of cell death is one of the fundamental cellular changes that contribute to malignant transformation in the tumor microenvironment [46, 48]. Rose linked apoptosis to tumor progression, the elimination of potentially malignant cells, and hyperplasia [35]. Furthermore, Rose noted that reduced apoptosis or its resistance plays a key role in carcinogenesis [35]. Previous studies have investigated different molecules and genes to explore the acquisition of resistance to apoptosis among tumor cells in the context of tumor evolution [35, 50]. To date, these molecules include the p53 tumor suppressor protein, proapoptotic Bcl-2 proteins, the Fas receptor, cytotoxic lymphocytes, and cellular FLICE-inhibitory protein (c-FLIP) [35, 50, 51, 52, 53]. In addition, evidence shows that the dynamics of somatic evolution and the process by which tumor cells acquire resistance to apoptosis are essential to the understanding, control, and management of cancer, as this process determines whether tumor cells will survive and proliferate in the tumor environment [49, 50].
A careful review of the existing evidence suggests that tumor cells can acquire and develop resistance to apoptosis in several ways [35, 50, 51]. One of the commonly discussed strategies leading to apoptotic resistance is the loss of p53 tumor suppressor protein function due to mutation. Liu, Zhang, and Feng noted that the p53 tumor suppressor protein is known to promote apoptosis by activating proapoptotic Bcl-2 proteins. Additionally, it was observed that p53 is a fundamental tumor suppressor due to its antioxidant defense mechanism and regulation of energy metabolism. Tumor-associated mutant p53 proteins not only lose their tumor suppressive function but also acquire oncogenic capabilities, such as the promotion of tumor cell survival and proliferation and the control of metabolic changes, metastasis, and angiogenesis [52, 53, 54]. Dysregulated death receptor pathways have also been linked to apoptosis resistance. For example, absence of the Fas receptor protects tumor cells from immune destruction mediated by cytotoxic lymphocytes. In other cases, overexpression of c-FLIP in cancer patients protects tumor cells from cytotoxic T cell-induced apoptosis [55, 56, 57].
Tumor evolution theory
The tumor evolution theory is a scientific theory postulating that natural selection exists and operates in any system consisting of components with different reproductive potentials [58, 59, 60]. The tumor evolution theory has been featured extensively in cancer literature and has been used to explain disease development and progression. Schwartz and Schäffer posit that cancer is a genetic disease characterized by the progressive accumulation and development of genomic aberrations that can be augmented by germline mutations [58]. Researchers have also argued that the accumulation of mutations in cancer patients is guided by evolutionary mechanisms and principles centered on the concepts of diversification and selection of mutations that facilitate tumor cell survival and proliferation [58, 59, 60, 61]. A critical review of a study conducted by Schwartz and Schäffer indicates that the evolutionary mechanism underlying cancer development and progression has become a fundamental guide to understanding, controlling, and predicting disease progression, therapeutic response, and metastasis [58].
The tumor evolution theory underscores the role of natural selection in cancer development [59, 60, 61, 62]. Coyle, Boudreau, and Marcato argued that in the context of cancer development, evolutionary progression of the disease or its reemergence after treatment involves cancer stem cells [62]. The authors noted that a widely accepted oncogenesis framework indicates that tumors typically originate from benign growths characterized by minor genetic alterations [62]. With time, genetic alterations such as the loss of heterozygosity, changes in copy number variation, microsatellite instability, and allelic imbalance accumulate, leading to aggressive cancers [62]. The continued accumulation of mutations allows tumor cells to invade various tissues and organs through metastasis. The fundamental biological properties of cancer cells include loss of sensitivity to programmed cell death and antigrowth signals, immortality, higher mutation rates, the capacity to attack tissues and cells through metastasis, altered metabolic properties, and the capacity to recruit blood vessels [62, 63]. Stem cells acquire these characteristics through evolution as they transform into cellular assailants that cannot be destroyed by the body's immune system [62, 63, 64].
In the case of cancer patients, selection favors the fittest stem cell variants that can survive and reproduce in the tumor microenvironment [9]. Greaves states that although any cancer cell can become a “fit” somatic cell variant, the effective units for selection are cell populations with sufficient genetic diversity and those with extensive self-renewal ability [9]. These two characteristics allow cancer cell populations to provide phenotypic substrates for evolutionary selection and propagate the selected traits to other cells and tissues [65, 66, 67].
Schwartz and Schäffer noted that the predominant mechanisms of cancer cell evolution and selection differ significantly from those associated with speciation. More specifically, the researchers observed that tumor evolution involves the selection of mutations that promote proliferation, survival, and other phenotypic characteristics and hallmarks of cancer stem cells, such as changes in copy number variation [58]. Notably, several recent studies have suggested that certain tumors and cancer stem cells evolve during neutral processes without undergoing the selection aspect of evolution. A study by Sottoriva et al., for example, illustrated that selective neutral mutations occur in the tumor microenvironment through genomic aberrations [20]. In their study, the genomes of 349 glands from 15 colorectal tumors were profiled to show that neutral mutations occur in cancer sites [20]. Nevertheless, Schwartz and Schäffer argued that selection plays a critical role in cancer development and progression by supporting the emergence of variants with desirable survival features, such as the loss of sensitivity to programmed cell suicide and antigrowth signals [20].
Vital discoveries have been made in the last decade, revealing the mechanism by which selection and evolution contribute to the emergence of tumor cell variants that are insensitive to the body's immune system. In addition, researchers have identified genes and molecules involved in tumor cell variation, including latent membrane protein (LMP) 2, LMP7, TAP, tapasin, BRCA1, and BRCA2 [58, 68, 69, 70]. A well-established mechanism by which selection contributes to the emergence of variant cells involves the downmodulation of antigen processing machinery, which in this case includes mutations that affect LMP 2, LMP7, TAP, and tapasin and downregulate tumor antigen expression [58, 68]. Downregulation of tumor antigen expression leads to enhanced metastasis and increased tumor incidence given that cytotoxic T lymphocytes (CTLs) will not recognize or respond to the targeted tumor cell antigens [69, 70]. The inability of CTLs to identify tumor antigens demonstrates that evolution and selection lead to the emergence of tumor variants that are resistant to the immune response, thereby supporting cancer progression.
Comparison of the theories
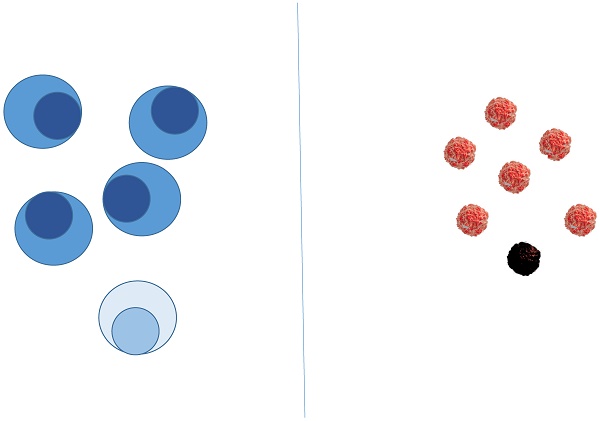
Burnet's clonal selection theory and the tumor evolution theory have been used in previous studies to examine the process of cancer development, progression, management, and control. A review of existing research shows that the two theories have some similarities. The fundamental similarity is that both Burnet's clonal selection theory and the tumor evolution theory strive to explore and explain the developmental process of cancer by focusing on mutations and replication. Second, the two theories use natural selection and survival of the fittest to show how tumors develop in cancer patients. Therefore, these theories provide insights into managing cancer and developing interventions for inhibiting tumor progression.
Notably, a review of previous studies shows that there are significant differences between Burnet's clonal selection theory and the tumor evolution theory. First, Burnet's clonal selection theory focuses on lymphocyte functions, specifically those in response to antigens that attack the body [32, 33]. In contrast, the tumor evolution theory underscores the significance of natural selection in cancer development [58, 59, 60]. Second, Burnet's clonal selection theory strives to explain how the immune system responds to infections and how it is related to tumor development, whereas the tumor evolution theory explains how fit somatic cell variants develop genetic diversity and how those with robust self-renewal ability develop in the tumor microenvironment [32, 33, 9].
Finally, Burnet's clonal selection theory emphasizes the role of B and T lymphocyte selection in the destruction of specific antigens [32, 33]. In contrast, the tumor evolution theory emphasizes the process and mechanisms by which selection and evolution lead to the emergence of tumor cell variants that are resistant to the immune response. Among the mechanisms that have been proposed to explain the development of such variants is the downmodulation of the antigen processing machinery, including LMP 2, LMP7, TAP, and tapasin [58, 68]. Table 1 summarizes the differences between Burnet's clonal selection theory and the tumor evolution theory.
Comparison of Burnets Clonal Selection Theory with the Tumor Evolution Theory
| Burnet's Clonal Selection Theory | Tumor Evolution Theory |
|---|---|
| Focuses on the functions of lymphocytes, specifically their response to antigens that attack the body | Focuses on the significance of natural selection in the development of cancers |
| Strives to explain how the immune system responds to infections and how it is related to tumor development | Strives to explain how fit somatic cell variants develop genetic diversity and how those with extensive self-renewal ability develop in the tumor microenvironment |
| Emphasizes the role of B and T lymphocyte selection in the destruction of particular antigens | Emphasizes the process and mechanisms by which selection and evolution lead to the emergence of tumor cell variants that are resistant to the immune response |
| Based on the expression and suppression of molecules such as p53 tumor suppressor protein, proapoptotic Bcl-2 proteins, the Fas receptor, cytotoxic lymphocytes, and cellular FLICE-inhibitory protein (c-FLIP) | Based on somatic mutations, such as mutations in LMP 2, LMP7, TAP, tapasin, BRCA1, and BRCA2 |
Consideration of mutations and errors
An important trait of biological systems is that they undergo mutations, thereby resulting in occasional errors. It is a hallmark of biological systems that changes, or mutations, will occur that will make occasional errors. Therefore, errors occur in biological systems. It is important to observe the errors that occur during tumorigenesis based on the tumor evolution theory and during clonal lymphocyte selection based on Burnet's clonal selection theory.
A) Occurrence of mutations and errors based on the tumor evolution theory
In general, the occurrence of mutations and the resulting errors depend on one of the basic principles of the theory of evolution applied in this field. Tumor cells change because mutations occur, resulting in errors and malfunctions. This change may decrease the survival likelihood of the resulting tumor cells and their daughter cells, eventually leading to cell death, or this change might confer a high chance of survival. In the latter case, tumor cells become more resistant, stronger, and capable of dividing faster; that is, their likelihood of survival increases. Changes to the structure of immunological receptors also enhance the survival of tumor cells. It is important to note that the immune system may not be able to eliminate the tumor cells once they begin to mutate; therefore, their likelihood of survival increases. In other words, mutation is the key mechanism for tumor cell survival.
B) Occurrence of mutations and errors based on Burnet's clonal selection theory
Errors are also likely to occur during the development and maturation of lymphocytes. The occurrence of such errors may cause mutations that may, in turn, change the structure of immune receptors. In most cases, a change in immune receptor structure results in the production of poorly functioning lymphocytes. In other words, the generation of a better-functioning lymphocyte appears to be unlikely via this random unplanned pathway. However, in some cases, improved lymphocyte binding may occur, and through proper selection, the numbers of these lymphocytes can be increased.
Synthesis of both components A (errors in tumor evolution) and B (errors in Burnet's theory)
Given that tumor cells are continuously mutating and changing, it may be pertinent to prevent the survival of a single lymphocyte with the best binding ability. In addition, the presence of several slightly mutated neighboring lymphocytes might also be relevant. In tumor cells that randomly undergo mutation, it may be useful to have a certain repertoire of similar receptor sequences available. When a mutation causes a sudden change in target structure, one of the neighboring lymphocytes that has a slightly different receptor sequence might be able to bind the mutated sequence and thus bring the tumor cell under control again; moreover, in the ideal case, that lymphocyte may even be able to destroy the tumor cell.
Thus, both systems—the potentially disease-causing oncogenic system and the tumor-controlling and -attacking immune system—are subject to the same molecular principles of evolutionary mutation and selection, and it is advantageous to allow lymphocytes with a nonoptimal binding structure to survive. It is not only reasonable to enable one of the lymphocytes with an optimal binding structure to propagate clones but also to advance the optimization of a single receptor that functions best at the molecular level. Moreover, it might be reasonable to consider potential changes in the target structure right from the outset, allowing a certain variance in receptor structure. We observed that allowing for errors and inaccuracies during lymphocyte selection might be useful. In fact, it might be beneficial to retain these errors from the outset. However, as stated above, although retaining lymphocytes with inaccurate binding might be considered advantageous, it is also potentially dangerous. By allowing inaccuracies in lymphocyte binding to occur, the possibility of cross-reactivity with endogenous structures is more likely. Thus, there is a tradeoff between the advantage of allowing inaccuracies to persist and the serious disadvantages that the inaccuracies may confer. For example, body structures may be attacked by the immune system or autoimmune diseases may develop.
Take-home messages
The development and modification of tumor cells and the maturation of lymphocytes are based on the same biological principles of mutation and selection. Within the framework of these biological principles, mild and heavy genetic mutations must be considered and are crucial for tumor development and control by lymphocytes. In some respects, the processes of tumor development and immune system development are distinct. Tumor cell evolution most often leads to tumor growth and metastasis, whereas evolution in the immune system attempts to attenuate tumor development.
Thus, we concluded that a certain degree of tolerance with regard to the accuracy of biological binding motifs and the target accuracy of immune cells (so-called biological variance) may be advantageous, as binding ability could be retained when a tumor cell begins to mutate. However, this biological variance in binding motifs is simultaneously potentially dangerous and can lead to the development of autoimmune diseases due to (A) an excessive level of immune cells or (B) unfortunate biological variance in binding motifs.
Conclusions
According to the above description and the literature, Burnet's clonal selection theory and the tumor evolution theory provide solid theoretical frameworks for understanding the dynamics of cancer development, progression, management, and control. These two theoretical frameworks use the concepts of natural selection, survival of the fittest, replication, and mutation to show how tumor cells acquire resistance to T and B lymphocytes. The selection process leads to the emergence of tumor cell variants that are insensitive to the immune response.
Consequently, future cancer immunotherapy studies should explore the distinct modes and pathways through which tumor cells evolve and develop resistance to lymphocyte action. Burnet's clonal selection theory and the tumor evolution theory provide a theoretical basis that researchers can use to discover and study antigen-receptor gene rearrangements, tolerance, and affinity maturation. By investigating possible sources of error, we conclude that it might be advantageous for the human body to allow a certain amount of biological variance in lymphocyte-binding receptors. However, it is important to note that the presence of this variance is also dangerous within the framework of autoimmune disease development.
Abbreviations
Bcl-2: B-cell lymphoma 2 protein; BRCA1: breast cancer 1 gene; BRCA2: breast cancer 2 gene; FAS-receptor: first apoptosis signal receptor; FLICE: FADD-like IL-1β-converting enzyme; FLIP: FLICE-like inhibitory protein; LMP 2: latent membrane protein 2; LMP7: latent membrane protein 7; p-53: p53 protein; TAP: transporter associated processing protein; Tapasin: TAP associated glycoprotein.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Torre L, Bray F, Siegel R, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics. CA: A Cancer Journal for Clinicians. 2015;65(1):87-108
2. Pattabiraman DR, Weinberg RA. Tackling the cancer stem cells-what challenges do they pose? Nature reviews Drug discovery. 2014;13(7):497-512
3. Chen F, Zhuang X, Lin L, Yu P, Wang Y, Shi Y. New horizons in tumor microenvironment biology: challenges and opportunities. BMC Medicine. 2015;13:45
4. Peske JD, Woods AB, Engelhard VH. Control of CD8 T-cell Infiltration into Tumors by Vasculature and Microenvironment. Advances in cancer research. 2015;128:263-307
5. Lv L, Pan K, Li X, She K, Zhao J, Wang W. et al. The accumulation and prognosis value of tumor infiltrating IL-17 producing cells in esophageal squamous cell carcinoma. PLoS ONE. 2011;6(3):e18219
6. Gajewski TF, Schreiber H, Fu Y-X. Innate and adaptive immune cells in the tumor microenvironment. Nature Immunology. 2013;14(10):1014-1022
7. Birbrair A, Zhang T, Wang Z, Messi M, Olson J, Mintz A, Delbono O. Type-2 pericytes participate in normal and tumoral angiogenesis. American Journal of Physiology: Cell Physiology. 2014;307(1):C25-C38
8. Janelle V, Langlois MP, Tarrab E, Lapierre P, Poliquin L, Lamarre A. Transient complement inhibition promotes a tumor-specific immune response through the implication of natural killer cells. Cancer Immunol Res. 2014;2(3):200-6
9. Greaves M. Evolutionary determinants of cancer. Cancer Discov. 2015;5(8):1-15
10. McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell. 2017;168(4):613-628
11. Delgado-SanMartin JA, Hare JI, de Moura AP, Yates JW. Oxygen-driven tumor growth model: A pathology-relevant mathematical approach. PLoS Comput Biol. 2015;11(10):e1004550
12. Varmus H, Kumar HS. Addressing the growing international challenge of cancer: a multinational perspective. Sci Transl Med. 2013;5(175):175
13. McGranahan N, Swanton C. Biological and therapeutic impact of intratumor heterogeneity in cancer evolution. Cancer Cell. 2015;27(1):15-26
14. Aparicio S, Caldas C. The implications of clonal genome evolution for cancer medicine. N Engl J Med. 2013;368(9):842-51
15. Murtaza M, Dawson S-J, Tsui DWY, Gale D, Forshew T, Piskorz AM, Parkinson C. et al. Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature. 2013;497(7447):108-12
16. Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6(224):224
17. Carreira S, Romanel A, Goodall J, Grist E, Ferraldeschi R, Miranda S. Tumor clone dynamics in lethal prostate cancer. Sci Transl Med. 2014;6(254):254
18. McGranahan N, Swanton C. Biological and therapeutic impact of intratumor heterogeneity in cancer evolution. Cancer Cell. 2015;27(1):15-26
19. Aparicio S, Caldas C. The implications of clonal genome evolution for cancer medicine. N Engl J Med. 2013;368(9):842-51
20. Sottoriva A, Kang H, Ma Z, Graham TA, Salomon MP, Zhao J. et al. A Big Bang model of human colorectal tumor growth. Nat Genet. 2015;47(3):209-16
21. Gerlinger M, Horswell S, Larkin J, Rowan AJ, Salm MP, Varela I. et al. Genomic architecture and evolution of clear cell renal cell carcinomas defined by multiregion sequencing. Nat Genet. 2014;46(3):225-33
22. Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N. et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6(224):224ra24
23. Carreira S, Romanel A, Goodall J, Grist E, Ferraldeschi R, Miranda S. et al. Tumor clone dynamics in lethal prostate cancer. Sci Transl Med. 2014;6(254):254ra125
24. de Bruin EC, McGranahan N, Mitter R, Salm M, Wedge DC, Yates L. et al. Spatial and temporal diversity in genomic instability processes defines lung cancer evolution. Science. 2014;346(6206):251-6
25. Ma Y, Dobbins SE, Sherborne AL, Chubb D, Galbiati M, Cazzaniga G. et al. Developmental timing of mutations revealed by whole genome sequencing of twins with acute lymphoblastic leukemia. Proc Natl Acad Sci. 2013;110(18):7429-33
26. Baca SC, Prandi D, Lawrence MS, Mosquera JM, Romanel A, Drier Y. et al. Punctuated evolution of prostate cancer genomes. Cell. 2013;153(3):666-77
27. Stephens PJ, Greenman CD, Fu B, Yang F, Bignell GR, Mudie LJ. et al. Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell. 2011;144(1):27-40
28. Shlien A, Campbell BB, de Borja R, Alexandrov LB, Merico D, Wedge D. et al. Combined hereditary and somatic mutations of replication error repair genes result in rapid onset of ultra-hypermutated cancers. Nat Genet. 2015;47(3):257-62
29. Aceto N, Bardia A, Miyamoto DT. et al. Circulating Tumor Cell Clusters are Oligoclonal Precursors of Breast Cancer Metastasis. Cell. 2014;158(5):1110-1122
30. Bettegowda C, Sausen M, Leary RJ. et al. Detection of Circulating Tumor DNA in Early- and Late-Stage Human Malignancies. Science Translational Medicine. 2014;6(224):224
31. Andor N, Maley C, Hanlee P. Genomic instability in cancer: teetering on the limit of tolerance. Cancer Res. 2017;77(9):OF1-OF7
32. Rose NR. Molecular mimicry and clonal deletion: a fresh look. Journal of Theoretical Biology. 2015;375:71-76
33. Dutton RW. In vitro studies of the antibody response: antibodies of different specificity are made in different populations of cells. Frontiers in Immunology. 2014;4(515):1
34. Redgrove KA, McLaughlin EA. The role of the immune response in chlamydia trachomatis infection of the male genital tract: A double-edged sword. Frontiers in Immunology. 2014;5:534
35. Rose N. Molecular mimicry and clonal deletion: A fresh look. Journal of Theoretical Biology. 2015;375(1):71-76
36. Belkaid T.W. Hand Y. Role of the microbiota in immunity and inflammation. Cell. 2014;157:121-141
37. Horai R, Silver PB, Chen J, Agarwal RK, Chong WP, Jittayasothorn Y. et al. Breakdown of immune privilege and spontaneous autoimmunity in mice expressing a transgenic T cell receptor specific for a retinal autoantigen. J Autoimmun. 2013;44:21-33
38. Horai R, Chong WP, Zhou R, Chen J, Silver PB, Agarwal RK, Caspi RR. Spontaneous ocular autoimmunity in mice expressing a transgenic T cell receptor specific to retina: A tool to dissect mechanisms of Uveitis. Curr Mol Med. 2015;15(6):511-6
39. Laan M, Peterson P. The many faces of aire in central tolerance. Frontiers in Immunology. 2013;4:326
40. Lin W, Cerny W, Chua E, Duan K, Yi J, Shadan N. et al. Human regulatory B cells combine phenotypic and genetic hallmarks with a distinct differentiation fate. J. Immunol. 2014;193(5):2258-2266
41. Stein-Streilein J, Caspi RR. Immune privilege and the philosophy of immunology. Frontiers in Immunology. 2014;5:110
42. Wirnsberger G, Hinterberger M, Klein L. Regulatory T-cell differentiation versus clonal deletion of autoreactive thymocytes. Immunol Cell Biol. 2011;89(1):45-53
43. MonteroJ DuttaC, van Bodegom D Weinstock D, Letai A. p53 regulates a non-apoptotic death induced by ROS. Cell Death and Differentiation. 2013;20(1):1465-1474
44. Braig F, Marz M, Schieferdecker A, Schulte A, Voigt M, Stein A. et al. Epidermal growth factor receptor mutation mediates cross-resistance to panitumumab and cetuximab in gastrointestinal cancer. Oncotarget. 2015;6(14):12035-12047
45. Carvalho J, Oliveira C. Extracellular vesicles—powerful markers of cancer evolution. Frontiers in Immunology. 2014;5:685
46. Dawson SJ, Rosenfeld N, Caldas C. Circulating tumor DNA to monitor metastatic breast cancer. N Engl J Med. 2013;369(1):93-94
47. de Bruin EC, McGranahan N, Mitter R, Salm M, Wedge DC, Yates L. et al. Spatial and temporal diversity in genomic instability processes defines lung cancer evolution. Science. 2014;346(6206):251-256
48. Diaz LA Jr, Williams RT, Wu J, Kinde I, Hecht J, Berlin J. et al. The molecular evolution of acquired resistance to targeted EGFR blockade in colorectal cancers. Nature. 2012;486(7404):537-540
49. Juan Liu, Cen Zhang, Zhaohui Feng. Tumor suppressor p53 and its gain-of-function mutants in cancer. Acta Biochim Biophys Sin (Shanghai). 2014;46(3):170-179
50. M Li Y-C, Wahl GM. MDM2, MDMX, and p53 in oncogenesis and cancer therapy. Nature Reviews Cancer. 2013;13(2):83-96
51. Valente L, Strasser A. Distinct target genes, and effector processes appear to be critical for p53-activated responses to acute DNA damage versus p53-mediated tumour suppression. BioDiscovery. 2013;8:3
52. Donzelli S, Fontemaggi G, Fazi F, Di Agostino S, Padula F, Biagioni F. et al. MicroRNA-128-2 targets the transcriptional repressor E2F5 enhancing mutant p53 gain of function. Cell Death and Differentiation. 2012;19(6):1038-1048
53. Neilsen PM, Noll JE, Mattiske S, Bracken CP, Gregory PA, Schulz RB, Lim SP. et al. Mutant p53 drives invasion in breast tumors through up-regulation of miR-155. Oncogene. 2013;32(24):2992-3000
54. Dong P, Karaayvaz M, Jia N, Kaneuchi M, Hamada J, Watari H. et al. Mutant p53 gain-of-function induces epithelial-mesenchymal transition through modulation of the miR-130b-ZEB1 axis. Oncogene. 2013;32(27):3286-95
55. Xue M, Pang H, Li X, Li H, Pan J, Chen W. Long non-coding RNA urothelial cancer-associated 1 promotes bladder cancer cell migration and invasion by way of the hsa-miR-145-ZEB1/2-FSCN1 pathway. Cancer Sci. 2016;107(1):18-27
56. Jiang FZ, He YY, Wang HH, Zhang HL, Zhang J, Yan XF, Wang XJ. et al. Mutant p53 induces EZH2 expression and promotes epithelial-mesenchymal transition by disrupting p68-Drosha complex assembly and attenuating miR-26a processing. Oncotarget. 2015;6(42):44660-74
57. Deng S, Li X, Niu Y, Zhu S, Jin Y, Deng S. et al. MiR-652 inhibits acidic microenvironment-induced epithelial-mesenchymal transition of pancreatic cancer cells by targeting ZEB1. Oncotarget. 2015;6(37):39661-75
58. Schwartz R, Schäffer AA. The evolution of tumor phylogenetics: principles and practice. Nature Reviews Genetics. 2017;18(1):213-229 doi:10.1038/nrg.2016.170
59. Naxerova K, Jain RK. Using tumor phylogenetics to identify the roots of metastasis in humans. Nat Rev Clin Oncol. 2015May;12(5):258-72
60. Altrock PM, Liu LL, Michor F. The mathematics of cancer: integrating quantitative models. Nat Rev Cancer. 2015;15(12):730-45
61. Beerenwinkel N, Schwarz RF, Gerstung M, Markowetz F. Cancer evolution: mathematical models and computational inference. Syst Biol. 2015;64(1):e1-25
62. Coyle K, Boudreau J, Marcato P. Genetic Mutations and Epigenetic Modifications: Driving Cancer and Informing Precision Medicine. BioMed Research International. 2017;2017(9620870):1-18
63. Kandoth C, McLellan M, Vandin F, Ye K, Niu B, Lu C. et al. Mutational landscape and significance across 12 major cancer types. Nature. 2013;502(7471):333-339
64. Nik-Zainal S, Davies H, Staaf J, Ramakrishna M, Glodzik D, Zou X. Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature. 2016;534(7605):47-54
65. Potter NE, Ermini L, Papaemmanuil E, Cazzaniga G, Vijayaraghavan G, Titley I. et al. Single-cell mutational profiling and clonal phylogeny in cancer. Genome Res. 2013;23:2115-25
66. Eirew P, Steif A, Khattra J, Ha G, Yap D, Farahani H. et al. Dynamics of genomic clones in breast cancer patient xenografts at single-cell resolution. Genome Res. 2013;23(12):2115-25
67. Piccirillo SGM, Colman S, Potter NE, van Delft FW, Lillis S, Carnicer M-J. et al. Genetic and functional diversity of propagating cells in glioblastoma. Stem Cell Reports. 2015;4(1):7-15
68. Johnson BE, Mazor T, Hong C, Barnes M, Aihara K, McLean CY. Mutational analysis reveals the origin and therapy-driven evolution of recurrent glioma. Science. 2014;343(6167):189-93
69. Kim TM, Jung SH, An CH, Lee SH, Baek IP, Kim MS. et al. Subclonal genomic architectures of primary and metastatic colorectal cancer based on intratumoral genetic heterogeneity. Nat Genet. 2016;48(7):768-76
70. Wang J, Cazzato E, Ladewig E, Frattini V, Rosenbloom DI, Zairis S, Abate F. Clonal evolution of glioblastoma under therapy. Nat Rev Cancer. 2015;15(12):730-45
Author contact
![]() Corresponding author: Borros Arneth, Institute of Laboratory Medicine and Pathobiochemistry, Molecular Diagnostics, University Hospital of the Universities of Giessen and Marburg UKGM, Justus Liebig University Giessen, Giessen, Germany, Feulgenstr. 12, 35392 Giessen, Germany. Tel. +49 641 985 41556; Fax. +49 641 985 55969; E-mail: borros.arnethmed.uni-giessen.de
Corresponding author: Borros Arneth, Institute of Laboratory Medicine and Pathobiochemistry, Molecular Diagnostics, University Hospital of the Universities of Giessen and Marburg UKGM, Justus Liebig University Giessen, Giessen, Germany, Feulgenstr. 12, 35392 Giessen, Germany. Tel. +49 641 985 41556; Fax. +49 641 985 55969; E-mail: borros.arnethmed.uni-giessen.de
 Global reach, higher impact
Global reach, higher impact