13.3
Impact Factor
Theranostics 2019; 9(14):4182-4191. doi:10.7150/thno.34411 This issue Cite
Research Paper
Determination of cerebrospinal fluid leakage by selective deletion of transferrin glycoform using an immunochromatographic assay
1. Department of Chemistry, School of Physics and Chemistry, Gwangju Institute of Science and Technology (GIST), Gwangju 500-712, Republic of Korea
2. Department of Chemical and Biological Engineering, Rensselaer Polytechnic Institute, Troy, NY, USA
3. Center for Biotechnology and Interdisciplinary Studies, Rensselaer Polytechnic Institute, Troy, NY, USA
4. Department of Chemistry and Chemical Biology, Rensselaer Polytechnic Institute, Troy, NY, USA
5. Division of Neurosurgery, Department of Neuroscience NYU-Winthrop Hospital, 259 1st St Mineola, NY 11501 and MD in Neurological Surgery P.C. Rockville Center, New York
Received 2019-2-25; Accepted 2019-4-13; Published 2019-5-31
Abstract
Cerebrospinal fluid (CSF) leakage can lead to brain and spine pathologies and there is an urgent need for a rapid diagnostic method for determining CSF leakage. Beta-2 transferrin (β2TF), asialotransferrin, is a specific CSF glycoprotein biomarker used to determine CSF leakage when distinguished from serum sialotransferrin (sTF).
Methods: We detected β2TF using an immunochromatographic assay (ICA), which can be potentially developed as a point-of-care (POC) testing platform. Sialic acid-specific lectin selectively captures sTF in multiple deletion lines within an ICA test strip, enabling the detection of β2TF. A sample pre-treatment process efficiently captures excess sTF increasing sensitivity for CSF leakage detection.
Results: An optimal cut-off value for determining the presence of CSF in test samples was obtained from receiver operating characteristic (ROC) analysis of the ratio of the test signal intensity and the deletion lines. On 47 clinical samples, ICA test strips discriminated CSF positive from negative samples with statistically significant (positive versus negative t-test; P =0.00027). Additional artificial positive samples, prepared by mixing CSF positive and negative clinical samples, were used as a further challenge. These positive samples were clearly discriminated from the negative samples (mixture versus negative t-test; P =0.00103) and CSF leakage was determined with 97.1% specificity and 96.2% sensitivity.
Conclusions: ICA represents a promising approach for POC diagnosis of CSF leakage. While requiring 70 min assay time inconvenient for POC testing, our method was significantly shorter than conventional electrophoresis-based detection methods for β2TF.
Keywords: cerebrospinal fluid leakage, transferrin, sialic acid, immunochromatographic assay, point of care testing
Introduction
Cerebrospinal fluid (CSF) leakage from the ear, nose, and other adjacent organs has been observed in nonsurgical traumatic (80%), surgical (16%) and non-traumatic (4%) modalities [1-3]. CSF has functions related to brain protection and untreated leakage can result in life-threatening meningitis, brain abscess, and pneumocephalus [4-6]. Thus, a rapid detection method for CSF leakage is critically needed. The confirmation of CSF leakage during surgery significantly impacts surgical decisions, and immediate repair of the defect is essential [3, 7]. Moreover, detection of spontaneous CSF leakage is extremely challenging, because CSF is a colorless fluid in humans and is difficult to distinguish when mixed with other biological fluids, such as serum. Furthermore, the symptoms of CSF leakage, including headache, tinnitus, and nasal drainage, are often misdiagnosed [3, 8-10]. Therefore, even a thorough medical examination based on limited external features can often fail to determine CSF leakage making additional and more definitive diagnostic methods necessary [11-13].
High-resolution computerized tomography (CT) and magnetic resonance imaging (MRI) are typically used to confirm the diagnosis of CSF leakage based on identifying the location of a defect [14, 15]. Imaging methods are accurate and precise; however, these tests are costly and require skilled operators and expensive equipment. CT and MRI are certainly not time or cost efficient and are rarely used on patients in preliminary examinations or during surgery. Currently, investigation of point-of-care (POC) tests, such as biochemical assays, are used in imaging pretesting for the initial detection of CSF leakage [16, 17]. Among these assays, the β2TF test is considered a reliable biochemical method for detecting CSF leakage [18-21]. Transferrin (TF) is a glycoprotein important for maintaining human iron homeostasis. TF is modified to β2TF (asialo-transferrin) in the CSF through the action of brain neuraminidase resulting in the elimination of terminal sialic acid residues on the glycan chains of TF, affording the β2TF glycoform constituting up to 30% of total CSF transferrin [22, 23]. Hence, the sensitive and reliable detection of β2TF is critical for determining CSF leakage.
Although the detection of β2TF has been used in the diagnosis of CSF leakage, there remain several practical limitations in using this method for a POC diagnosis. The minor differences in the TF-based glycan chains make it difficult to distinguish β2TF from sialo transferrin (sTF) since sTF is a major component in serum. Currently, these TF glycoforms are distinguished using electrophoresis, requiring a relatively long processing time (120-150 min), and skilled professionals for highly reproducible diagnosis of CSF leakage [24, 25]. Moreover, an electrophoresis-based assay is usually performed in remote highly specialized professional clinical laboratories that requires additional turnaround time for sample analysis [26]. Thus, conventional electrophoresis for detecting β2TF is unsuitable as a POC assay for rapid diagnosis and immediate treatment of CSF leakage. These considerations provide strong motivation for developing a new rapid assay for the determination of β2TF in the diagnosis of CSF leakage.
Only two studies have been reported for the rapid detection of β2TF for determining CSF leakage. Papadea and Schlosser [27] reported the detection of β2TF using an immunofixation electrophoresis system and this is not a rapid method of analysis. This system could reproducibly separate β2TF from sTF and provide sensitive detection within 2.5 h. Kwon et al. [28] selectively eliminated sTF using a chemical and enzymatic method allowing the rapid detection of CSF leakage. In this study, sTF was treated with an enzyme to covalently couple it to micron sized magnetic beads, which were then removed using a magnetic separator, and the residual β2TF was quantitatively analyzed using an enzyme-linked immunosorbent assay (ELISA). Unfortunately, both of these approaches still required considerable time and multiple laborious process steps to detect CSF leakage.
Herein, we report the detection of β2TF using an immunochromatographic assay (ICA), which has the potential to serve as a low cost POC testing platform with rapid and easy to perform operation. In this ICA method, sialic acid-specific lectin is immobilized into multiple deletion lines at the beginning of a test strip to capture sTF, and anti-transferrin antibodies are immobilized in a detection line near the end of the test strip. Thus, the serum specific sTF is selectively captured early in the deletion lines, allowing β2TF to move alone along the test strip to the detection line. In addition to the enhanced efficiency of sTF capture by sialic acid-specific lectin, a sample pre-treatment process step was also used to eliminate the binding of other unidentified sialo glycoproteins and the hook effect, which results in a higher likelihood for false negatives despite high concentrations of analyte [29]. Mixtures of CSF and serum were next analyzed using our newly developed method, and correlated values obtained between signal intensity of the test and deletion lines were compared on the basis of mixing ratios of CSF (%) and serum. Finally, 47 clinical samples were evaluated using this method, and significant differences were observed between the positive samples, negative samples, and artificial mixtures. Receiver operating characteristic (ROC) analysis was performed to obtain the optimal cut-off value based on Youden's index [30], from which we could determine whether the test samples contained CSF.
Materials and Methods
Materials
Surfactant 10G (95R-103) and bovine serum albumin (BSA) were from Fitzgerald Industries International (Acton, MA, USA). Anti-transferrin monoclonal antibody (4T15-8B9; conjugated Ab, 4T15-11D3; immobilized Ab) was obtained from Hytest (Joukahaisenkatu, Turku, Finland). Neo protein saver (NPS-301) was obtained from Toyobo (Satte City, Kamiyoshiba, Japan). Spin column tubes (69725), and spin desalting columns (89891) were purchased from Thermo Fisher Scientific (Waltham, MA, USA). G1 reaction buffer (B1723) was from New England Biolabs (Ipswich, MA, USA). Sambucus nigra lectin (L-1300) and biotinylated S. nigra lectin (B-1305) were from Vector laboratories (Burlingame, CA, USA). Centrifugal filters (UFC510096), laminated cards (HF000MC100) and the nitrocellulose (NC) membrane (HFB01804) were from Millipore (Billerica, MA, USA). Sample and absorbent pads (Grade 222) were sourced from Bore da Biotech (Seongnam-si, Gyeonggi-do, Korea). Gold colloidal solution was from BBI International (EM.GC20; Cardiff, UK). Polyvinylpyrrolidone (PVP 29K), transferrin (T8158), neuraminidase (N2876), human serum (H4522), sodium metaperiodate (S1878), streptavidin (S4762), and other chemicals were from Sigma-Aldrich (St. Louis, MO USA). All buffers and reagent solutions were prepared using distilled water generated using an ELGA water purification system (Lane End, UK).
Antibody oxidation
Sialic acid residues on the glycan chains of the anti-transferrin antibody were oxidized to reduce antibody binding to the sialic acid-specific lectin. Antibody (1 mg mL-1) was treated with 1 mM sodium metaperiodate in acetate buffer solution (0. 1 M, pH 5.5). After incubation at 4 ºC for 30 min, the sodium metaperiodate was removed using desalting resin-based centrifugation at 1,000 × g for 3 min at 4 ºC. The desalting resin was prepared in a spin column tube with 750 µL after washing with 1 × phosphate-buffered saline (PBS) and centrifugation three times at 1,000 × g for 3 min at 4 ºC. After desalting, the diluted antibody solution was replaced by washing with 1 × PBS using a centrifugal filter at 12,000 × g for 20 min at 4 ºC. The antibody was then bound to BSA (Mr = 66 kDa) using a BSA antibody ratio of 1:10 for 90 min at 25 ºC. After the BSA treatment, unbound BSA was removed by centrifugal ultrafiltration (MWCO 100 kDa) with 1 × PBS at 12,000 × g for 20 min at 4 ºC. After filtration, the antibody-BSA complex was diluted with 1 × PBS to 1 mg mL-1 based on the initial amount of antibody. This treated antibody is designated as oxidized-antibody.
Preparation of streptavidin-gold nanoparticle (AuNP) conjugate
Streptavidin (10 μL, 1 mg mL-1) was added to a mixture of 1 mL of 20 nm colloidal gold nanoparticles (AuNP, 1 OD) and 100 μL of borate buffer (0.1 M, pH 8.4). After incubation at room temperature (RT, 25 °C) for 30 min, 100 μL Neo protein saver (50 mg mL-1) was added to this mixture to block the residual sites on the surface of the AuNPs. After incubation at 4 °C for 60 min, the mixture was centrifuged using a refrigerated micro centrifuge (Smart R17; Hanil Science Industrial Co., Gangwon-do, Korea) at 13,475 × g for 20 min at 10 °C. The supernatant was discarded, the AuNP conjugates were re-suspended in 10 mM borate buffer (pH 8.4), and the centrifugation and re-suspension steps were repeated twice. The final re-suspended AuNP conjugate solution was concentrated 2-fold by changing the solution volume to 1 × PBS containing 50 mg mL-1 trehalose, 5 mg mL-1 neo protein saver, 2 mg mL-1 Tween 20, and 10 mg mL-1 Triton-X 100. Prior to using the AuNP-streptavidin conjugate, the solution was diluted with the same volume of 1 × PBS solution.
Preparation of ICA test strip
The ICA test strip was assembled from an NC membrane, absorbent pad, and sample pad. The non-oxidized anti-transferrin antibody (11D3) was immobilized (8 mm from beginning on the top side of the NC membrane; 30 × 2.5 cm2) using a dispenser (DCI 100; Zeta Corporation, Kyunggi-do, Korea). The antibody-loaded NC membrane was dried in a chamber at 37 °C and 15% humidity for 15 min. After incubation, the absorbent pad (Grade 222; 30 × 2 cm2) was attached to the top and bottom side of the NC membrane with a 2 mm overlap. The combined NC membrane and absorbent pad was cut into 4 mm wide strips using a cutting machine.
Evaluation of lectin specificity
Three ICA test strips with loaded oxidized and non-oxidized anti-transferrin antibodies were prepared to evaluate the specificity of lectin for sTF and the results obtained by oxidizing the antibody. One pair each of the three ICA test strips loaded with oxidized and non-oxidized anti-transferrin antibodies were dipped into the sTF, β2TF, and control solution for 15 min. β2TF was prepared by reacting sTF (100 µg mL-1) with a neuraminidase (10 µg mL-1) in 1 × G1 reaction buffer overnight at 37 °C. We prepared the sTF (1 µg mL-1), β2TF (1 µg mL-1), and control solution (no protein) based on the loading buffer that contains 1 × PBS with PVP (10 mg mL-1) and surfactant 10G (5 mg mL-1). Subsequently, the ICA test strips were dipped in the loading buffer and washed for 5 min. After washing, the ICA test strips were dipped into biotinylated sialic acid-binding lectin solution (10 µg mL-1) in the loading buffer for 15 min. The ICA test strips were then washed with the same solution for 15 min. The ICA strips were dipped into the prepared AuNP-streptavidin conjugate solution for 15 min and washed with loading buffer. The color signal intensity was measured using the image analyzing equipment (ChemiDoc TM XRS+ Imaging System; Bio-Rad Laboratories, Hercules, CA, USA). The captured image was analyzed using the Image Lab 4.0 software (Bio-Rad). The colorimetric signal intensities were analyzed with the profiling of the line for each strip sensor, compensating for the background signal intensity of the NC membrane. Subsequent signal intensity analyses were performed using the same method.
Determination of effect of sample pretreatment
Oxidized anti-transferrin antibody-AuNP conjugate was prepared using the same method used for streptavidin, except that the final re-suspension solution was also replaced with 10 mM borate buffer solution (pH 8.5). The ICA test strips were also prepared using the same method with the control line immobilized at 4 mm from the end on the top side of the NC membrane and the five deletion lines immobilized at 12, 14, 16, 18, and 20 mm from the end on the top side of the NC membrane. The pooled serum and CSF solutions were diluted from 20-fold to 20,000-fold with 1 × PBS containing PVP (10 mg mL-1) and surfactant 10G (5 mg mL-1). For sTF and β2TF, similar concentrations of pooled serum and CSF were spiked in 1 × PBS containing PVP (10 mg mL-1) and surfactant 10G (5 mg mL-1) based on the comparison of the titration curve results in the buffer-spiked assay (see Figure S1 in the online Data Supplement). Furthermore, 100 µL of each prepared solution was applied to the prepared ICA test strips and for assays using sample pretreatment, the pooled serum and CSF were reacted with the AuNP conjugate for 15 min. In addition, the solution was purified three times by centrifugation at 13,475 × g for 15 min at 10 °C and applied to the ICA test strips. After 8 min, 1 × PBS containing PVP (10 mg mL-1) and surfactant 10G (5 mg mL-1) was applied to the sample pad, and then the results were analyzed using the method described in the previous section.
Application of mixed samples
The pooled serum and CSF were mixed in ratios of 1:3, 1:1, and 3:1. The mixed sample and pooled serum and CSF (20-fold dilution) were reacted with 1 × AuNP conjugate for 15 min and purified three times by centrifugation at 13,475 × g for 15 min at 10 °C. The purified solutions were then applied to the ICA test strips and analyzed using the method previously described. For the assay using 10% and 30% serum samples, the serum was diluted with 1 × PBS and the same process was repeated.
Evaluation of clinical samples
We obtained 47 clinical samples were from Neurological Surgery, P.C. Rockville Centre, NY, USA (13 positive and 34 negative samples). Since these samples were destined for disposal and de-identified, IRB approval was not required. An additional 13 artificially mixed samples were prepared by mixing the same volume of 13 positive samples and 13 randomly selected negative samples. The serum samples were stored at -80 °C for subsequent analysis. The clinical samples were also evaluated using the same method used for the mixed samples described above. As standard reference methods to evaluate clinical samples, the beta-2 transferrin was predetermined by the diagnostic service company (Quest Diagnostics Inc., NY) [31].
Results and Discussion
Detection strategy and ICA design
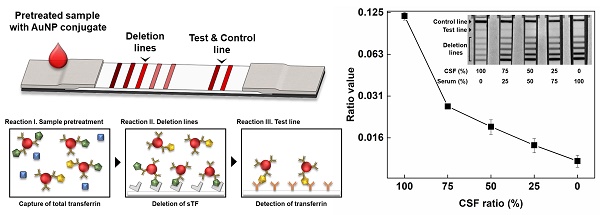
The β2TF assay for determining of CSF leakage require the distinguishing the glycan chain between β2TF and sTF. The glycan chains of β2TF in CSF have different terminal sugar residues than are found on the glycan chains of serum specific-sTF due to the action of a brain neuraminidase. Hydrolysis of TF glycan chains by this neuraminidase removes their non-reducing terminal sialic acid residues resulting in generation of the β2TF (asialo-transferrin) glycoform. Thus, the glycan chains of CSF β2TF differ from those of sTF in which all of its glycan chains are capped with terminal sialic acid residues. Based on the specificity of a sialic acid-binding lectin, we designed a detection strategy for the diagnosis of CSF leakage (Figure 1). In the first step of the sample pretreatment process (Figure 1A), the sample solutions are treated with an anti-transferrin (TF) antibody (Ab), specific for transferrin, which are then conjugated to gold nano particle (AuNP), thereby capturing total TF (sTF + β2TF). The pretreated sample containing TF-AuNP complexes is then loaded onto the ICA test strip (Figure 1B). On the ICA test strip, proximal to the loading position, there are multiple deletion lines, containing sialic acid-specific lectin, and further downstream a test line, containing an anti-TF antibody, and close to the end of the test strip, a control line with anti-mouse IgG antibody that serves as a positive control. To demonstrate the strategy, we evaluated the specificity of sialic acid binding lectin, improved deletion efficiency through sample preparation and applied our assay to mixture samples, prepared with CSF and serum, and 47 clinical samples.
The reactions taking place in sample pre-treatment, the deletion lines, and the test line are illustrated in Figure 1C. During the sample pretreatment process, both β2TF and sTF are captured by the anti-TF Ab-AuNP conjugates and these complexes are recovered by centrifugation. Next, this pretreated solution containing the TF-AuNP complexes is loaded onto the ICA sample pad and then migrated along the test strip towards the absorbent pad (Figure 1B). The TF-AuNP complexes differentially bind to the specific sialic acid-binding lectin immobilized in the deletion lines, which selectively remove sTF-AuNP complexes but allow the β2TF AuNP complexes to proceed along the test strip. These β2TF (asialo-transferrin)-AuNP complexes flow forward encountering the test line where they are captured with immobilized anti-TF antibody, resulting in a detection signal at the test line. The signal intensity at the test line serves as an indicator of the amount of β2TF in a given sample. The control line indicates the performance of ICA works well.
Evaluation of the specificity and efficiency of lectin in the deletion lines of the ICA test strip
The specificity and the efficiency of the sialic acid-binding lectin in the capture of sTF at the deletion lines on the ICA test strip is critical for a successful CSF leakage diagnostic. Hence, the specificity of sialic acid-binding lectin for sTF capture was evaluated using a NC membrane dipstick method. Anti-TF antibodies were immobilized on a NC membrane strip and the strips were dipped into the solutions containing sTF, β2TF, and PBS (negative control), respectively, followed by the sequential binding of biotinylated lectin and streptavidin-AuNP conjugate to these NC strips. This experiment confirmed the binding of sTF to the sialic acid-binding lectin. However, the results also showed weak signal for both β2TF and the control (Figure 2A). We hypothesized that this unexpected signal resulted from the interaction of the anti-transferrin Ab with the sialic acid-binding lectin. This lectin interaction might result from the glycan chains of antibody that also can contain terminal sialic acid residues. The mild periodate oxidation of the anti-transferrin antibody removes the terminal sialic acid residues from its glycan chains leaving aldehyde groups in these glycan chains [32]. The use of oxidized antibodies (asialo-Ab) greatly reduced the undesired interaction between anti-transferrin Ab and the sialic acid-binding lectin (Figure 2A). Thus, the periodate oxidation of this antibody improved the selectivity of the interaction between sialic acid-binding lectin and sTF by avoiding removing the interaction of β2TF-anti-transferrin antibody AuNP conjugate (Figure 2B) with only a relatively small loss of sTF signal intensity.
Schematic illustration of detection strategy of beta-2 transferrin (β2TF) for determination of cerebrospinal fluid (CSF) leakage. (A) Sample pretreatment process, (B) structure of immunochromatographic assay (ICA), and (C) reaction mechanisms of the entire process.
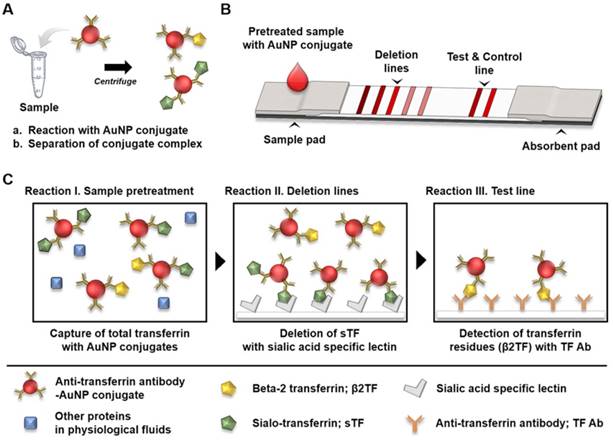
Demonstration of specificity of lectin in immunochromatographic assay (ICA) by evaluation of (A) oxidation effect of antibody. (B) Comparison of colorimetric signal intensity between sialo-transferrin (sTF), beta-2 transferrin (β2TF), and control.
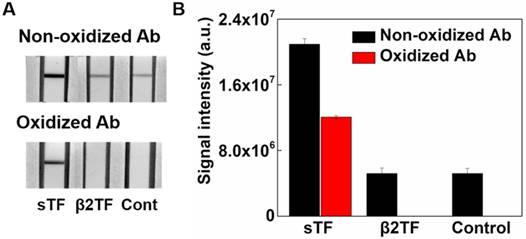
Next, we evaluated the efficiency of the deletion lines in the ICA test strip using serum and CSF. The concentrations of TF in both serum and CSF were first quantified using the ICA test strip after preparing different concentrations of TF spiked-buffer solutions. We compared the signal intensity of these TF solutions, CSF, and serum in the test lines in the ICA strip (Figure S1 in the online Data Supplement). The results showed that the concentration of TF in serum and CSF was approximately 2 mg mL-1 and 20 µg mL-1, respectively. Based on these concentrations we also prepared the sTF-spiked and β2TF-spiked PBS solutions and adjusted the concentration of sTF (2 mg mL-1) to be comparable to that of serum and the concentration of β2TF (20 µg mL-1) to be comparable to that of CSF. Different concentrations of the sTF-spiked, β2TF-spiked buffer solution, serum, and CSF were each applied to the ICA test strips (Figure 3). The results showed no detectable signal in the deletion lines over the range of 20- to 200-fold diluted serum but signal was observed in the deletion lines over the range of 2,000- to 20,000-fold diluted serum. In the sTF-spiked PBS signals were detected in the deletion lines over the range of 200- to 20,000-fold dilution. These results showed that the serum required a 20,000-fold dilution to completely remove the sTF. However, in the case of both sTF spiked in buffer and serum the deletion lines on the ICA test strip (Figure 3A) were non-functional at 20-fold dilution due to the hook effect [29].
After quantifying the signal intensity in the five different deletion lines in each diluted sample containing sTF, the sTF-spiked PBS solutions (1 µg mL-1) showed similar pattern, that has decreasing deletion proportion from forward along to rear line, as observed for the pretreated serum samples which contained 100 µg mL-1 of sTF, while the 2,000-fold diluted serum, despite which contained 1 µg mL-1 of sTF, showed an inverted pattern (Figure S2 in the online Data Supplement). These results provide evidence of the presence of unidentified sialo glycoproteins in serum that compete for the binding of TF-AuNP conjugates to the sialic acid-binding lectin immobilized in the deletion lines. Therefore, it is clear that the sample pretreatment process is required for efficient elimination of these unidentified and interfering sialo glycoproteins. In addition, the sample pretreatment process can also eliminate the hook effect caused by excess amounts of unconjugated TF that competes with the TF-AuNP conjugates for binding to the sialic acid-binding lectin immobilized in the deletion lines, resulting in decreased signal in the deletion lines.
In the case of CSF, the lectin immobilized in the deletion lines successfully captured sTF over the entire dilution range (20- to 20,000-fold) tested, as the total protein concentration in CSF is considerably lower than that of serum (Figure 3A). A signal for the test line could be observed for CSF over the range of 20- to 2,000 fold dilution of CSF samples; however, there was no detectable signal using 20,000 fold-diluted CSF (Figure 3C). These results suggest that a > 20,000-fold dilution of serum was required for the complete removal of sTF but that CSF solutions should be diluted < 20,000-fold to detect β2TF at the test line (Figure 3B and C). A pretreatment process, therefore, was required to overcome the discordance between these dilution factors for serum and CSF and to eliminate the undesired interfering sialo glycoproteins competing with sTF for the sialic acid-binding lectin immobilized in the deletion lines. The results showed that the pretreated serum and CSF solutions afforded increased signals in the deletion lines over the entire range of dilutions (Figure 3). In addition, no hook effect was observed for the pretreated serum and CSF samples (Figure 3A).
Evaluation of CSF content with the ICA strip
The ICA test strip containing five deletion lines and a test line was developed for detecting the presence of CSF in test samples (Figure 1). The complete removal of sTF with a sialic acid-specific lectin immobilized in five deletion lines was essential for good detection sensitivity of CSF leakage. Various unidentified sialo-glycoproteins in human fluids resulted in unacceptable false-negatives, since these sialo-glycoproteins also bind to the sialic acid-specific lectin. Thus, a sample pretreatment process was required to eliminate interfering glycoproteins and the unconjugated TF that could compete with binding of sTF-AuNP complexes to the sialic acid-binding lectin immobilized in the deletion lines. Although this pretreatment process increased the efficiency for the sTF removal by the sialic acid-binding lectin on the five deletion lines (Figure 3), there were several additional limitations for the accurate detection of CSF. First, the anti-TF Ab-AuNP conjugates could bind to both sTF and β2TF simultaneously [33]. Second, the physiological concentration of sTF in the serum was approximately 100-fold higher than that in CSF. Third, β2TF constitutes only ~30% of the total TF in the CSF [34, 35]. Taking these limitations into consideration, the binding of sTF to the anti-TF Ab-AuNP conjugates should dominate those of β2TF. As a result, the sTF-β2TF-AuNP complexes are captured in the deletion lines. Hence, the signal of β2TF in test line might not be sufficient for detection despite the presence of CSF. Furthermore, all of the sTF in test sample might not be captured by the sialic acid-binding lectin in the deletion lines because of the short reaction time on the ICA test strip or because of the weak interaction between sialic acid-binding lectin and glycoprotein [36], resulting in the detection of a false positive signal in the test line due to sTF instead of β2TF. Finally, because the concentration of TF in test fluids from human body are variable [37-39], we need to measure not only the β2TF captured at a test line, but also the sTF captured with the lectin in deletion lines in order to accurately determine CSF leakage. Therefore, the ratio of the signal intensity of test line (for β2TF) to the signal intensity of deletion lines (sTF) were determined and the ratio (signal of a test line divided by the signal of the sum of deletion lines) must be determined to overcome these limitations.
(A) Evaluation of efficiency of deletion lines, sensitivity of test lines and effect of sample pretreatment process (C stands for control line, T: test line, and D: deletion lines), (B) the comparison of sum of colorimetric signal intensity of deletion lines, and (C) signal intensity of test line.
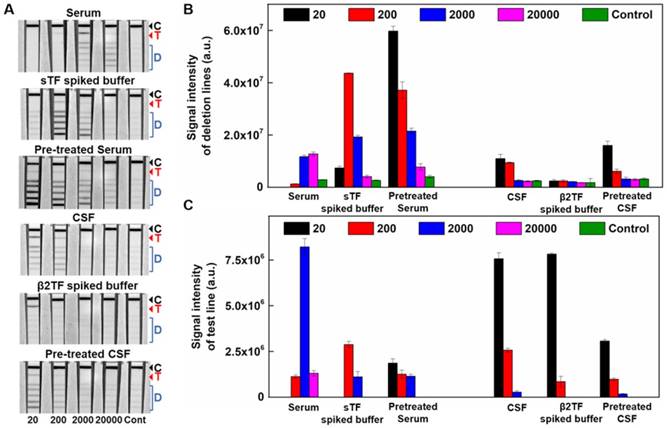
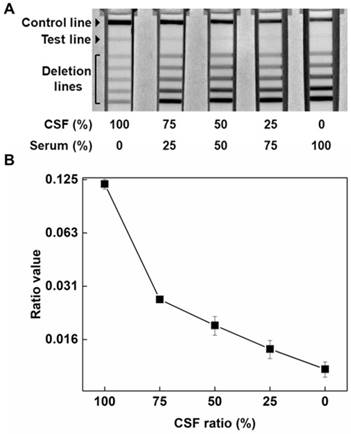
To address these issues, we prepared different mixtures of pooled serum and CSF, and the mixtures were applied to the ICA test strips after sample pretreatment. As shown in Figure 4A, as the percentage in the mixture of CSF decreased, the signal intensity at the test line decreased, and in contrast, the sum of the signal intensity in the deletion lines increased (Figure S3 in the online Data Supplement). These results suggest that the proportion of sTF and β2TF in each sample depend on the mixture ratio of CSF and serum used in a test sample. By considering the signals in both the deletion lines and test line, we could obtain a ratio (signal intensity of the test line / the sum of signal intensities of the deletion lines). These ratios were proportional to the content of CSF in the mixtures (Figure 4B). In addition, we also evaluated mixtures of CSF and diluted serum (10% and 30% diluted in PBS) to mimic various body fluids, such as otorrhea, rhinorrhea and drainage from the spinal suture area. The results of these experiments showed that the ratio also proportionally increased with an increased content of CSF (Figure S4 in the online Data Supplement). In conclusion, the use of both sample pretreatment and a ratio that takes into account signals in both the test line and deletion lines were essential for accurate determination of CSF leakage using the ICA test strip.
Performance of immunochromatographic assay (ICA) used for mixed sample based on (A) cerebrospinal fluid (CSF) proportion and (B) the ratio value (the signals of a test line divided by the signals of the sum of deletion lines) using test and deletion lines.
Evaluation of clinical samples
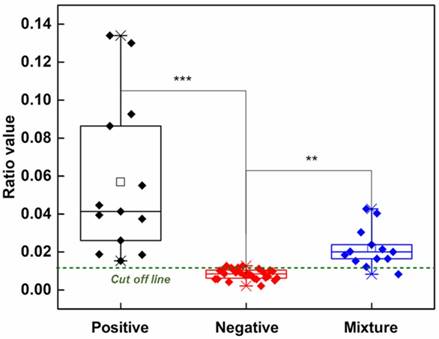
We next analyzed 47 clinical samples (13 positive and 34 negative samples) obtained from brain ventricular, lumbar wound, cervical wound and postoperative drainage from spinal surgery (see Table S1 in the online Data Supplement). Because the positive samples contained over 90% CSF, the ICA test strips could easily discriminate positive samples, containing CSF, and negative samples, (positive versus negative t-test; P=0.00027 in Figure 5). We next prepared 13 additional artificial positive samples by mixing positive clinical samples, containing CSF, with randomly selected negative samples to further challenge our ICA method. The artificial positive mixtures were again clearly discriminated from the negative samples (mixture versus negative t-test; P = 0.00103 in Figure 5).
Comparison of the ratio value (the signals of a test line divided by the signals of the sum of deletion lines) between clinical samples (positive n = 13, negative n = 34, artificial mixture = 16, *** stands for p value < 0.001, ** for <0.01)
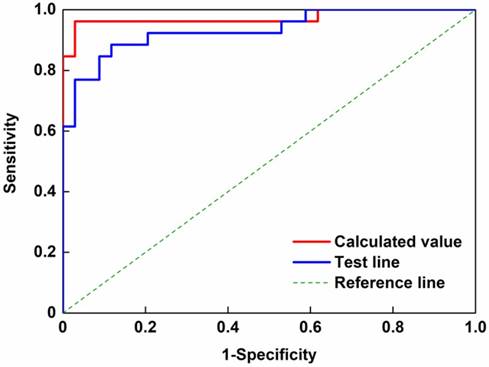
Because the number and diversity of our samples were insufficient to evaluate the performance of our newly developed method, we further evaluated the performance of our ICA method based on a ROC curve using two parameters (the ratio value and signal intensity of the test line in Figure 6). In these analyses the artificial mixtures were included in the positive sample group. The area under the curve (AUC) values indicated the effectiveness of the ICA test strip method in distinguishing the positive and negative samples, were 0.9728 and 0.9333 for the ratio value and test line signal intensity, respectively [40]. AUC values range from perfect discrimination (AUC = 1) and no discrimination (AUC = 0.5) between the positive and negative samples. Thus, our newly developed ICA method was significantly capable of distinguishing positive samples from negative samples. Furthermore, we calculated the Youden's index (J) [30] from the ROC curve, which can be used for obtaining an optimal cut-off value. Based on this value, the specification of the developed method was evaluated and is summarized in Table S2 in the online Data Supplement. Based on the Youden's index and AUC value, we confirm that the ratio value was more valid than the signal intensity of the test line, although by combining the quantification of detection signals obtained from the ICA test strip with statistical analysis, we were able to determine CSF leakage with 97.1% specificity and 96.2% sensitivity.
Conclusion
In conclusion, we have developed a novel POC method for determining CSF leakage by detecting β2TF using an ICA test strip. To test the effectiveness of this approach, we analyzed 47 clinical samples and 13 artificial mixtures prepared from positive and negative samples. We could clearly discriminate between the positive and negative samples (t-test; P=0.00027). ROC analysis indicated that our method can be used for the determination of CSF leakage. The Youden's index of the ROC was used to define the optimal cut-off value, and the specificity and sensitivity were 97.1% and 96.2%, respectively. However, our method requires an extended assay time (70 min) mainly because of the sample pretreatment process (60 min), which is critical because of considerable interference caused by other sialo-glycoproteins present and the high concentration of TF in human fluids. However, when compared to conventional electrophoresis-based detection methods for β2TF, the entire assay time of our method was significantly shorter and could be better adapted to a POC device. We anticipate that our ICA test strip method might also be applicable to the detection of other biomarkers containing (a)sialo-glycoproteins.
Receiver operating characteristic (ROC) analysis of clinical samples based on parameter of immunochromatographic assay (ICA) for determination of cerebrospinal fluid (CSF) leakage
Abbreviations
AUC: area under the curve; AuNP: gold nanoparticle; β2TF: Beta-2 transferrin; CSF: cerebrospinal fluid; CT: computerized tomography; ELISA: enzyme-linked immunosorbent assay; ICA: immunochromatographic assay; MRI: magnetic resonance imaging; POC: point of care; ROC: receiver operating characteristic; sTF: sialo transferrin; TF: transferrin.
Supplementary Material
Supplementary figures and tables.
Acknowledgements
This research was supported by Global Research Laboratory Program (2014K1A1A2043032), the Brain Research Program (2015M3C7A1029196) and the Mid-career Researcher Program (2017R1A2B3010816) through a National Research Foundation (NRF) grant funded by the Ministry of Science, ICT, and Future Planning.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Friedman JA, Ebersold MJ, Quast LM. Post-traumatic Cerebrospinal Fluid Leakage. World J Surg. 2001;25:1062-1066
2. Loew F, Pertuiset B, Chaumier E, Jaksche H. Traumatic, spontaneous and postoperative CSF rhinorrhea. Adv Tech Stand Neurosurg. 1984;11:169-207
3. Prosser JD, Vender JR, Solares CA. Traumatic cerebrospinal fluid leaks. Otolaryngol Clin North Am. 2011;44:857-873
4. Sakka L, Coll G, Chazal J. Anatomy and physiology of cerebrospinal fluid. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:309-316
5. Suliman S, Gurlek A, Byrne J, Sullivan N, Thanabalasingham G, Cudlip S. et al. Nonsurgical cerebrospinal fluid rhinorrhea in invasive macroprolactinoma: incidence, radiological, and clinicopathological features. J Clin Endocrinol Metab. 2007;92:3829-3835
6. Zada G, Lopes MBS, Mukundan S, Laws E. Spontaneous, Traumatic, and Postoperative CSF Rhinorrhea. Atlas of Sellar and Parasellar Lesions. cham: Springer. 2016:517-523
7. Abuabara A. Cerebrospinal fluid rhinorrhoea: diagnosis and management. Med Oral Patol Oral Cir Bucal. 2007;12:397-400
8. Fiky LE, Kotb A, Mostafa BE. A Unified Management for Spontaneous CSF Leak. International Int J Otorhinolaryngol Head Neck Surg. 2015;4:141-147
9. Ricketti AJ, Cleri DJ, Porwancher RB, Panesar M, Villota FJ, Seelagy MM. Cerebrospinal fluid leak mimicking allergic rhinitis. Allergy Asthma Proc. 2005;262:125-128
10. Schievink WI. Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol. 2003;60:1713-1718
11. Oudart J-B, Zucchini L, Maquart F-X, Dubernard X, Labrousse M, Fiabane G. et al. Tau protein as a possible marker of cerebrospinal fluid leakage in cerebrospinal fluid rhinorrhoea: A pilot study. Biochem Med. 2017;27:1-5
12. Schievink W, Maya M, Louy C, Moser F, Tourje J. Diagnostic criteria for spontaneous spinal CSF leaks and intracranial hypotension. AJNR Am J Neuroradiol. 2008;29:853-856
13. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-2296
14. Lloyd KM, DelGaudio JM, Hudgins PA. Imaging of skull base cerebrospinal fluid leaks in adults. Radiology. 2008;248:725-736
15. Vemuri NV, Karanam LS, Manchikanti V, Dandamudi S, Puvvada SK, Vemuri VK. Imaging review of cerebrospinal fluid leaks. Indian J Radiol Imaging. 2017;27:441
16. Mantur M, Łukaszewicz-Zając M, Mroczko B, Kułakowska A, Ganslandt O, Kemona H. et al. Cerebrospinal fluid leakage—Reliable diagnostic methods. Clin Chim Acta. 2011;412:837-840
17. Ziu M, Savage JG, Jimenez DF. Diagnosis and treatment of cerebrospinal fluid rhinorrhea following accidental traumatic anterior skull base fractures. Neurosurg Focus. 2012;32:E3
18. Chan DT, Poon WS, Ip CP, Chiu PW, Goh KY. How useful is glucose detection in diagnosing cerebrospinal fluid leak? The rational use of CT and Beta-2 transferrin assay in detection of cerebrospinal fluid fistula. Asian J Surg. 2004;27:39-42
19. Nandapalan V, Watson I, Swift A. Beta-2-transferrin and cerebrospinal fluid rhinorrhoea. Clin Otolaryngol. 1996;21:259-264
20. Ryali RG, Peacock MK, Simpson DA. Usefulness of β2-transferrin assay in the detection of cerebrospinal fluid leaks following head injury. J Neurosurg. 1992;77:737-739
21. Warnecke A, Averbeck T, Wurster U, Harmening M, Lenarz T, Stöver T. Diagnostic relevance of β2-transferrin for the detection of cerebrospinal fluid fistulas. Arch Otolaryngol Head Neck Surg. 2004;130:1178-1184
22. Brown KJ, Vanderver A, Hoffman EP, Schiffmann R, Hathout Y. Characterization of transferrin glycopeptide structures in human cerebrospinal fluid. Int J Mass Spectrom. 2012;312:97-106
23. Hoffmann A, Nimtz M, Getzlaff R, Conradt HS. 'Brain-type'N-glycosylation of asialo-transferrin from human cerebrospinal fluid. FEBS Lett. 1995;359:164-168
24. Görögh T, Rudolph P, Meyer JE, Werner JA, Lippert BM, Maune S. Separation of β2-transferrin by denaturing gel electrophoresis to detect cerebrospinal fluid in ear and nasal fluids. Clin Chem. 2005;51:1704-1710
25. McCudden CR, Senior BA, Hainsworth S, Oliveira W, Silverman LM, Bruns DE. et al. Evaluation of high resolution gel β2-transferrin for detection of cerebrospinal fluid leak. Clin Chem Lab Med. 2013;51:311-315
26. Hawkins RC. Laboratory turnaround time. Clin Biochem Rev. 2007;28:179
27. Papadea C, Schlosser RJ. Rapid method for β2-transferrin in cerebrospinal fluid leakage using an automated immunofixation electrophoresis system. Clin Chem. 2005;51:464-470
28. Kwon SJ, Zhang F, Dordick JS, Sonstein WJ, Linhardt RJ. Detection of cerebrospinal fluid leakage by specific measurement of transferrin glycoforms. Electrophoresis. 2015;36:2425-2432
29. Tate J, Ward G. Interferences in immunoassay. Clin Biochem Rev. 2004;25:105
30. Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biometrical Journal: Biom J. 2008;50:419-430
31. Schnabel C, Di Martino E, Gilsbach JM, Riediger D, Gressner AM, Kunz D. Comparison of beta2-transferrin and beta-trace protein for detection of cerebrospinal fluid in nasal and ear fluids. Clin Chem. 2004;50:661-663
32. Hermanson GT. Bioconjugate Techniques. 3rd Ed. San Diego, CA: Elsevier Inc. 2013
33. Sotnikov DV, Radchenko AS, Zherdev AV, Dzantiev BB. Determination of the composition and functional activity of the conjugates of colloidal gold and antibodies. Eurasian J Anal Chem. 2016;11:169-179
34. Earley CJ, Connor J, Beard J, Malecki E, Epstein D, Allen R. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology. 2000;54:1698-1700
35. Kasvosve I, Delanghe J. Total iron binding capacity and transferrin concentration in the assessment of iron status. Clin Chem Lab Med. 2002;40:1014-1018
36. Lu Y-W, Chien C-W, Lin P-C, Huang L-D, Chen C-Y, Wu S-W. et al. BAD-lectins: boronic acid-decorated lectins with enhanced binding affinity for the selective enrichment of glycoproteins. Anal Chem. 2013;85:8268-8276
37. Firkin F, Rush B. Interpretation of biochemical tests for iron deficiency: diagnostic difficulties related to limitations of individual tests. Aust Prescr. 1997;20:74-76
38. Tolosano E. Increasing serum transferrin to reduce tissue iron overload due to ineffective erythropoiesis. Haematologica. 2015;100:565-566
39. Vatutin M, Smyrnova G, Shevelyok A, Kashanska O, Sklyanna O, Keting O. Differential diagnosis of anemia in patients with rheumatoid arthritis. Arch Rheumatol. 2014;29:042-6
40. Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4:627
Author contact
![]() Corresponding authors: M.G.K.: Fax: +82-62-715-3419, E-mail address: mkimac.kr; R.J.L.: Fax: +1-518-276-3405, E-mail address: linharedu
Corresponding authors: M.G.K.: Fax: +82-62-715-3419, E-mail address: mkimac.kr; R.J.L.: Fax: +1-518-276-3405, E-mail address: linharedu
 Global reach, higher impact
Global reach, higher impact